In July, MVC hosted two virtual workgroup presentations – the first, a rural health workgroup focused on how a sepsis compliance initiative was developed and implemented in a critical access hospital setting. The second, a post-discharge follow-up workgroup, presented a small acute care hospital’s journey to patient satisfaction excellence. The MVC Coordinating Center hosts workgroup presentations twice per month, covering a variety of topics including post-discharge follow-up, sepsis, cardiac rehab, rural health, preoperative testing and health in action.
Rural Health Workgroup July 8, 2025
MVC hosted a rural health workgroup with a presentation by Victoria Durr, BSN, RN, Infection Prevention Coordinator from Scheurer Health. The presentation spotlighted a targeted sepsis compliance initiative and shared key strategies, lessons learned, and outcomes tailored to rural healthcare.
Meeting sepsis bundle compliance requirements set by the Centers for Medicare & Medicaid (CMS) is not only vital for reimbursement and regulatory alignment but also directly tied to improved patient mortality outcomes. As Durr explained, rural hospitals face unique challenges to improving sepsis compliance including agency coverage, fewer staff, and limited diagnostic tools.
As a part of her initial assessment of SEP-1 bundle compliance at Scheurer Health, Durr evaluated her staff’s understanding of the sepsis bundle components and found significant knowledge gaps. Other challenges faced by Schurer Health included limited space to admit directly from the emergency department (ED), an inconsistent sepsis census, and changing admitting privileges. These challenges contribute to downstream impacts to sepsis compliance including limited staff awareness and training, changes to lab orders, and transitions in continuity of care.
In July of 2024, Durr began working through each issue one-by-one with the help of department leadership. She outlined specific strategies Scheurer Health has used to improve compliance including:
- Implementation of structured training and process changes to standardize sepsis detection across emergency, inpatient, and inpatient care units
- Employed a team-based strategy, pairing clinicians and quality improvement leads to reinforce consistent sepsis protocols across inpatient workflows
- Leveraged data analytics to identify gaps and monitor compliance in real time
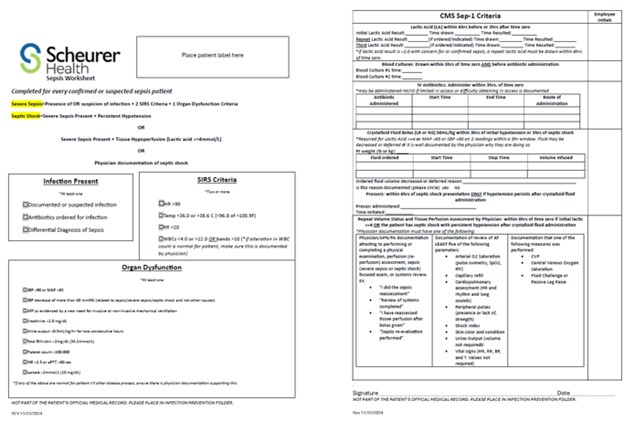
One key proactive tool Durr developed was a step-wise sepsis worksheet for nursing staff to follow in the case of a sepsis patient (see Figure 1, access PDF here). While this form is not required, in those cases when it has been utilized, Durr has found 100% SEP-1 compliance. A similar summary guide was created for physicians to optimize work flows (see PDF here).
Figure 1. Step-Wise Sepsis Worksheet for Nursing
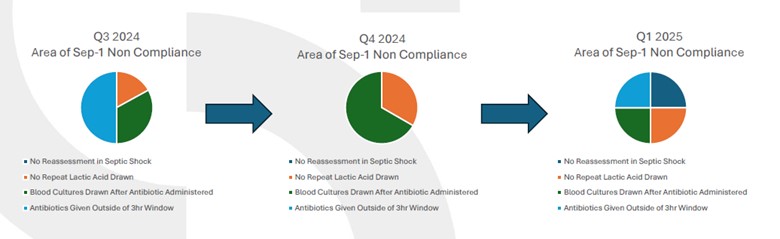
While Durr notes she has only evaluated data for sepsis cases dating back to July of 2024, she has seen a shift in the areas of SEP-1 non-compliance over time. Analysis revealed that some areas of non-compliance have improved while others have worsened (Figure 2). For example, between Q3 2024 and Q4 2024, non-compliance with antibiotic delivery within a three-hour window significantly declined, while non-compliance with blood cultures being drawn after antibiotic administration increased. However, by Q1 2025 when almost all the strategies outlined above had been implemented, the distribution of SEP-1 non-compliance areas became relatively even. Durr notes that real-time tracking has allowed her team to pinpoint manageable areas of improvement and inform their next steps.
Figure 2. Tracking Areas of SEP-1 Non-Compliance
In the future, Durr notes Scheurer Health will continue to improve SEP-1 compliance through the implementation of a SEP-1 orientation with newly hired ED and acute care unit nurses, the creation of a standardized nurse handoff report, and continued tracking and team report outs on various metrics including length of stay (LOS), mortality, and sepsis related readmissions.
The workgroup presentation and follow-up discussion not only emphasized specific challenges to improving SEP-1 compliance at a rural health center but also offered solutions. Some of the solutions shared with attendees included recommendations to:
- Standardize workflows and checklists to build consistency across units
- Create on-demand education modules
- Utilize checklists available through the electronic medical records (EMR)
- Optimize nursing and physician champions
- Use data dashboards for real-time feedback
Rural Health Workgroup July 8, 2025 Recording
Post Discharge Follow Up Workgroup July 24, 2025
MVC’s second workgroup in July featured a presentation by Sara Hagerman BSN, RN, Quality Performance Improvement Specialist for University of Michigan Health-Sparrow at the Clinton, Carson, and Lansing sites. The presentation outlined the various pathways UMH Sparrow Carson has taken to improve their Hospital Consumer Assessment of Healthcare Providers and Systems survey (HCAHPS) scores.
HCAHPS is a tool developed by CMS that measures patient satisfaction. The survey consists of 27 questions that measure different aspects of patient care, including communication with providers, hospital environment, medication management, transitions from hospital to home care, and discharge planning. The survey is administered at various points throughout a patient’s stay, and results are used to compare hospitals on a national level.
Hagerman explains that starting about one year ago, the University of Michigan Health-Sparrow Carson devised a plan to not only improve HCAHPS scores but also to decrease readmissions. To do this, they focused on three primary areas:
- Evaluation of social determinates of health (SDoH)
- Individualized discharge planning
- Care facilitator follow-up
After collecting SDoH metrics in the Electronic Health Record (EHR) for about a year, the team aggregated this data to determine the greatest needs within their patient population. They also specifically looked for corresponding readmission cases to determine if readmissions were contributed to by social needs. Hagerman notes they found food insecurity (3.9%), housing instability (4.2%), and transportation needs (3.9%) to be the most common social factors impacting their community.
Transitioning from a micro to a macro-level, University of Michigan Health-Sparrow Carson senior executives next worked with their community partners to support improved transportation and food assistance resources at the local level. They collaborated with local programs to identify new resources for transportation and food assistance and developed pathways to connect patients directly with these resources prior to discharge.
With these resources in place, the team turned to tailoring individualized patient discharge plans. At UMH Sparrow Carson, nearly 90% of patients discharged have a scheduled follow-up appointment with their primary care provider (PCP) prior to leaving the hospital. And for those without a confirmed PCP, teams set a goal to follow-up within 3-7 days or less. Other components of the individualized discharge plans include:
- Review of SDoH screening and arrangement for appropriate support services
- Review of home care instructions, medications, and patient education
- Post-discharge contact information and call-back within 72 hours
Lastly, Hagerman described the third component of their program triad: care facilitators. Care facilitators are nurses embedded in primary care offices whose primary goal is to identify and support chronically ill patients. They can support care transitions, medication management, patient education, and enhance overall experience. Care facilitators can also enroll patients in UMH Sparrow’s Chronic Care Management Program.
Benefits to enrollment in the Chronic Care Management Program include improved care coordination, increased patient engagement, and reduced hospitalizations. Hagerman points to a readmission rate of 5.9% thus far in 2025, compared to a readmission rate in 2024 of 6.95% as evidence of the positive impact this program has had. However, Hagerman notes there are limitations to the availability of this program to patients due to the cost of patient copays.
When it comes to improving HCAHPS scores, Hagerman noted that perhaps the most important lesson learned in this process has been to ensure team members are aware of the content of HCAHPS surveys. “It’s important to understand what patients will be asked about in order to better address potential issues up front”, noted Hagerman and she’s encouraged her team to become more knowledgeable about the survey. Additionally, engaging an interdisciplinary team and sharing data is especially useful to ensure communication and continued progress. The UMH Sparrow Carson leadership team meets in person at their strategy huddle board every other week to discuss progress and next steps (Figure 3).
Figure 3. Tier 2 Strategy Huddle Board
Post Discharge Follow Up Workgroup July 24, 2025 Recording
MVC’s July workgroups specifically highlighted successful quality initiatives at small rural and acute care hospitals in Michigan. Their insights provide a basic understanding of the unique struggles these hospitals face to implement and maintain quality improvement.
MVC welcomes workgroup presenters from across Michigan to share their expertise, successes, initiatives and solution-focused ideas with fellow MVC members. Interested in presenting? Please reach out to us by email or submit a presentation proposal here.




