On April 16, 2025, MVC hosted a virtual networking event providing members with an opportunity to make professional connections and discuss strategies for improving post-discharge follow-up for sepsis patients. Forty-six MVC members from thirty-three hospitals and seven health systems participated in the ninety-minute event.
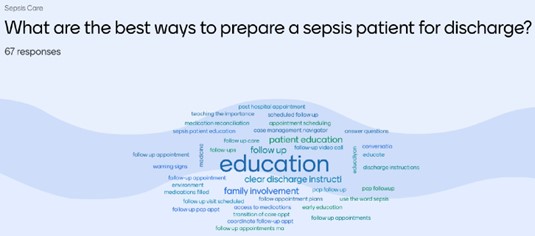
The event kicked off with an ice breaker activity (Figure 1) and an interactive quiz on common sepsis patient demographics, symptoms, and discharge care best practices.
Figure 1. Best Ways to Prepare a Sepsis Patient for Discharge Poll
Prior to starting the breakout discussion groups, MVC’s Engagement Manager, Jessica Souva, MSN, RN, C-ONQS presented unblinded hospital-level 14-day follow-up after sepsis rates for 30-day inpatient episodes from July 1, 2023, to June 30, 2024.
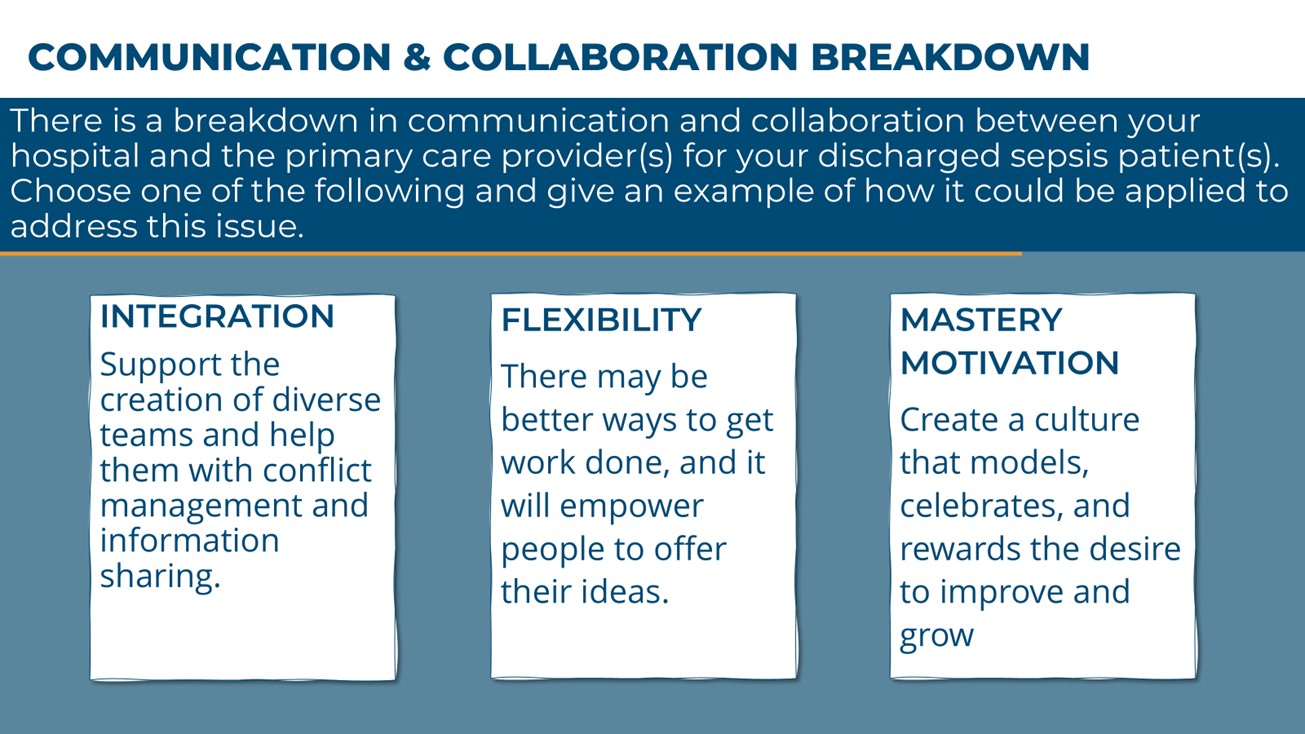
The breakout discussions were structured to engage attendees in conversations about challenges and strategies to addressing barriers in patient follow-up after sepsis. This goal was accomplished by providing groups with specific scenarios and types of approaches to improve follow-up after discharge for sepsis patients (Figure 2).
Figure 2. Challenges and Strategies to Address Barriers in Patient Follow-Up After Sepsis
What challenges are MVC members facing related to follow-up after discharge for sepsis patients?
MVC members reported that sepsis patients often face challenges in scheduling follow-up appointments, not knowing when to contact their provider for early warning signs and being readmitted before their scheduled post-discharge follow-up appointments. Contributing factors include lack of provider ability, incomplete patient or family education, and sub-optimal discharge dispositions.
What are MVC members doing to improve their rates of follow-up after discharge for sepsis patients?
During the breakout discussions, attendees shared that they are addressing the identified challenges through a multifaceted approach focusing on patient education, communication, resource access, team collaboration, and data evaluation.
Patient Education and Empowerment
- Discharge Paperwork: Include a phone number for patients to call with questions or concerns and to schedule follow-up appointments. This allows patients to seek follow-up care sooner.
- Family Involvement: Educate and involve family members to facilitate follow-up care by ensuring they understand the importance.
- Empowering Survivor Stories: Share stories from patient survivors through interviews, surveys, or patient advisory councils. These stories can be used to educate current patients, their families, and providers.
Communication and Coordination
- Care Coordinator/Nurse Navigator: Assign a care coordinator or nurse navigator as the point of contact post-discharge. Care Coordinators and Nurse Navigators can help patients understand factors influencing readmission and how to mitigate these factors.
- Continuous Communication: Maintain open communication between inpatient and outpatient case managers regarding transitions of care.
- “Call Back Crew”: Build a team to follow up with patients, reinforce education, and use call centers to identify trends and improve follow-up processes.
Resource Access
- Scheduling Follow-Up Appointments: When possible, schedule follow-up appointments before discharge.
- Discharge Clinics: Block time for a dedicated provider to staff a clinic for patients who do not have or are unable to get an appointment with their PCP. This type of clinic can reduce return ED visits and readmissions by providing support, education, and resources.
- Educate Staff About Under-utilized Resources: Local Area Agencies on Aging can facilitate access to free or low-cost services to improve the home setting for patients aged 65+. Many insurance providers, like Medicare Advantage/BCBSM provide additional support post-discharge with designated case managers.
Team Collaboration and Internal Processes
- Multi-Disciplinary Approach: Include care management and various therapies to support patient recovery. Ensure all patients receive a physical and occupational therapy evaluation to screen basic functional needs before discharge and determine the best future care setting.
- Unified Team Message: Ensure therapy, physician, and care management teams provide a unified message to patients.
- Improve Team Reliability and Training: Build internal trust and, consequently, patient trust. Provide physicians with training on how to conduct difficult discussions with patients and their families, ensuring patients understand their situation and the benefits of alternative approaches when recommended by medical professionals.
Data and Evaluation
- Patient Interviews and Surveys: Include a readmission nurse on the patient care team to interview readmitted patients and learn from their experiences. The readmission nurse can act as a liaison between quality and hospital care teams, highlighting patients needing special attention and collecting feedback.
- Retrospective Review: Complete a retrospective review of the patient’s journey to identify improvements needed in education and communication upon readmission for the same reason.
- Care Transition Programs: Add sepsis patients to Care Transition Programs to trigger alerts for retrospective review of readmission cases and to identify improvement areas.
What are members saying about the MVC April Virtual Networking Event?
- “Very fun and informational event. I like the smaller break out sessions to foster meaningful conversation and then bringing the ideas of the smaller groups to the entire group.”
- “Very well organized. I loved the interactive piece.”
- “I enjoyed the pre-break out group survey/quiz questions to help with engagement…it is less intimidating to speak up in the smaller groups than when everyone is in on large group.”
- “I enjoyed the networking aspect of this event and look forward to others in the near future. MVC Site Engagement Coordinators did a wonderful job facilitating this event and engaging the participants.”
- “It was reassuring to hear that many of the hospitals across the state are having the same issues and working on similar projects. It gave me a sense that my own hospital is on the right path.”
MVC looks forward to hosting more virtual networking events throughout the year to increase collaboration and connection with MVC’s members. If your hospital or organization has a networking topic they would like to share, please email us. We would love to hear from you.




