One of the most prevalent comorbidities in the United States is diabetes; as many as 1 in 10 Americans are diagnosed with this condition, and 90-95% having potentially preventable Type 2 diabetes. It is well documented that unstable blood glucose levels can contribute to increases in morbidity, mortality, and healthcare costs.
In the inpatient setting, the current standard of care for monitoring and testing blood glucose levels in diabetic patients is point-of-care (POC) testing, which combines a specific testing schedule and approved devices to measure blood glucose levels. A recent study involving 110 adults with Type 2 diabetes looked at implementing real-time continuous glucose monitoring (RT-CGM) in order to better manage inpatient glycemic levels. The patients were on a non-intensive care unit (ICU) floor, and received either the standard of care or the RT-CGM with Dexcom G6 monitoring—where a tiny sensor wire is inserted just beneath a person’s skin using an automatic applicator. Data was transmitted from the bedside wirelessly, and monitored by hospital telemetry. The bedside nurses were notified of any abnormal glucose levels or trends and the patients were treated accordingly. The results indicated that patients in the RT-CGM group demonstrated lower mean glucose levels and less time in hyperglycemia.
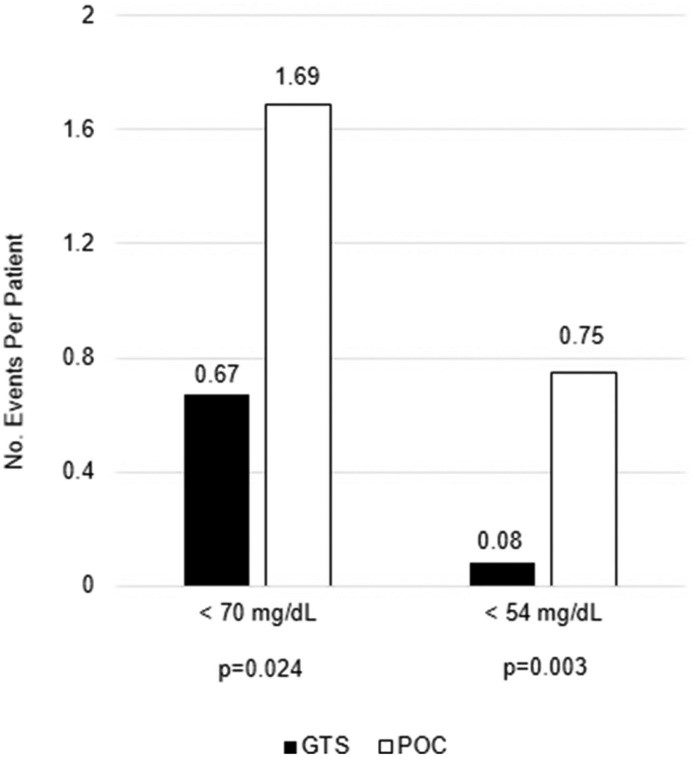
Another study that evaluated the efficacy of RT-CGM discussed the effect that uncontrolled glycemic levels can have on clinical outcomes and healthcare costs. Currently, hospitals use POC glucose testing in order to monitor and treat hypoglycemia, and it is recommended that POC testing occur four to six times per day. However, this leaves many hours throughout the day where hypoglycemia can go undetected. RT-CGM using a glucose telemetry system (GTS) offers an alternative method to monitor these glucose values. A total of 82 patients participated in this study. Patients in the RT-CGM group experienced 60.4% fewer hypoglycemic events compared to the POC group. Figure 1 below illustrates the number of hypoglycemic events per patient for both the CGM/GTS and the POC.
Figure 1.
RT-CGM has yet to be implemented in inpatient settings for several reasons. The primary reason is the lack of U.S. Food and Drug Administration (FDA) approval. Additionally, institutional challenges may act as a significant barrier. For instance, staff need to be prepared for increased workload and educated on appropriate protocols and procedures. Technological support is required to ensure hardware compatibility and maintain a robust internet network with minimal interference in transmission of results and alerts. Additional factors within the hospital setting include certain medications, procedures, nutrition, acute illness, and any other condition that may affect glucose control. All of these challenges have the potential to impact CGM and its associated workload because of the effect they may have on the patients’ blood glucose levels. Although challenges remain to the implementation of RT-CGM in the inpatient setting, the benefits may outweigh the risks; thus, it is worth considering, especially given the successes in the outpatient arena.
The Michigan Value Collaborative hosts diabetes workgroups where topics such as continuous glucose monitoring are discussed by Collaborative members. If you are interested in attending the next MVC diabetes workgroup, please connect with the MVC Coordinating Center at: michiganvaluecollaborative@gmail.com.