The birth of a child is a life-changing experience and a significant clinical event, with those experiencing pregnancy and childbirth hoping for a positive experience and healthy outcome. Yet the maternal mortality rate in the United States was 23.8 per 100,000 live births in 2020, and four in five pregnancy-related deaths were preventable according to the CDC. One in four of these deaths occur on the day of delivery or within one week, with considerable evidence that negative outcomes are more likely for patients of color. These findings are evidence of the need for quality improvement initiatives that ensure all people who are pregnant or postpartum receive the care they need. In light of this, the Michigan Value Collaborative (MVC) recently collaborated with the Michigan Health and Hospital Association (MHA) Keystone Center on the development of a statewide report on birth outcomes.
MVC claims data comprise approximately 84% of Michigan's insured population; these data are processed into 30- and 90-day price-standardized and risk-adjusted episodes of care that allow MVC to identify practice variation and measure the value of care. MVC creates episodes for over 40 medical and surgical conditions, including vaginal and cesarean childbirth delivery. MVC used a subset of claims from its data on Michigan childbirth episodes to create this new statewide report. The goal was to highlight statewide disparities in care and support the MHA Keystone Center and the Michigan Alliance for Innovation on Maternal Health (MI AIM) in their efforts to increase equitable care and decrease preventable severe maternal morbidity and mortality in Michigan.
MVC’s new statewide childbirth episodes report provides information on total episode payments, mode of delivery, patient characteristics, and rates of certain birth-related complications using 90-day episodes of care for vaginal and cesarean delivery. Measures in this report are based exclusively on Blue Cross Blue Shield of Michigan (BCBSM) PPO Commercial episodes for childbirth index admissions that occurred at MVC-participating hospitals between 1/1/19 and 12/31/21. Hospitals in this report were unidentified and each was required to have a minimum of 20 childbirth episodes across the reporting period to be included. Similarly to other MVC reports, several metrics were displayed by the index hospital’s geographic region of Michigan as categorized by MVC (see MVC regions here), with others stratified by race or mode of delivery.
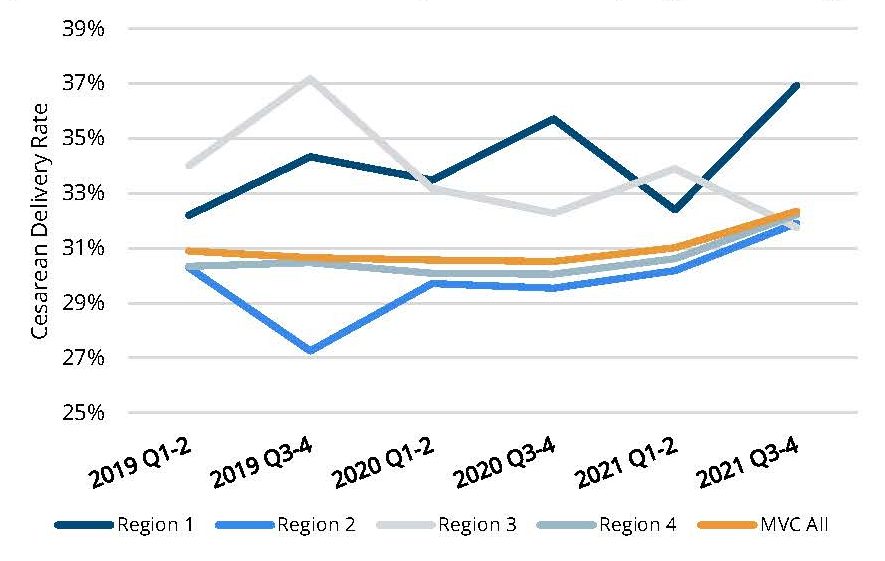
The analysis found an average price-standardized, risk-adjusted 90-day total episode payment of $7,765 for vaginal delivery and $10,264 for cesarean delivery (Figure 1), with average index lengths of stay of 3.1 and 4.0 days, respectively. Additionally, the overall rate of cesarean delivery was 32.3% in July-Dec. of 2021, a slight increase compared to cesarean rates in 2019 and 2020 (Figure 2).
Figure 1. Average Price-Standardized and Risk-Adjusted 90-Day Total Episode Payments by Mode of Delivery, Overall and by Hospital
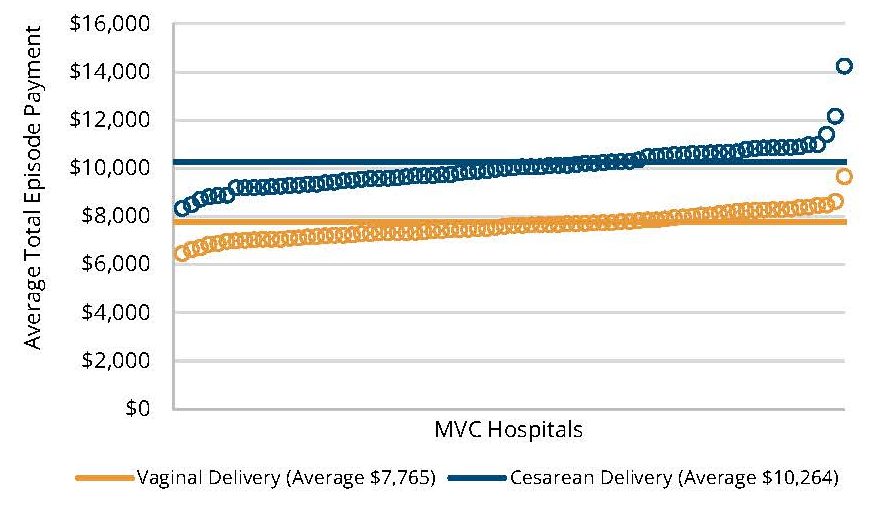
Figure 2. Rates of Cesarean Delivery, 2019 Through 2021, Overall and by Region of Michigan
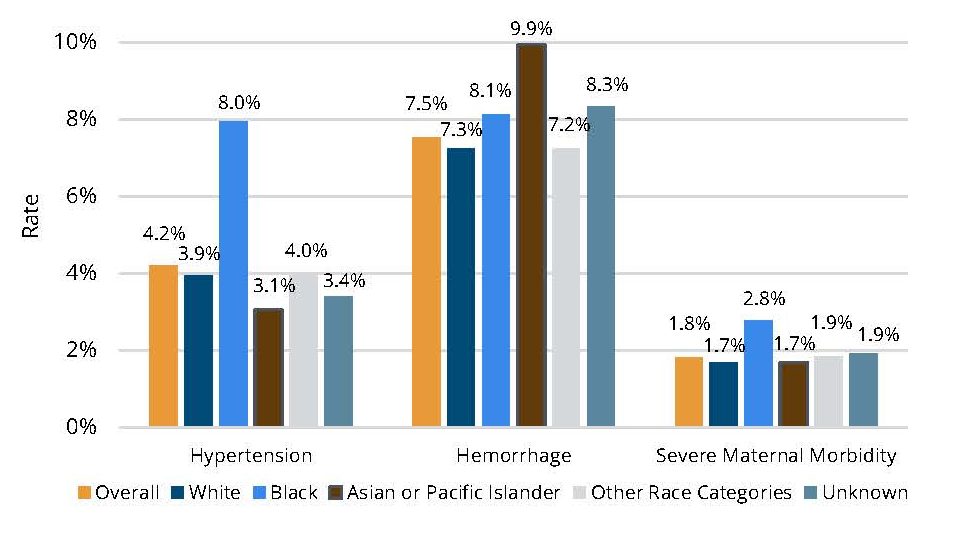
Overall, 7.5% of patients had a diagnosis of hemorrhage, 4.2% had a diagnosis of hypertension, and 1.8% had a diagnosis of severe maternal morbidity (SMM) during their index birth hospitalization. A notable finding was the difference in rates of these complications by race (Figure 3). Patients who were identified as Asian or Pacific Islander had higher rates of hemorrhage than other race categories, and patients who were identified as Black had higher rates of hypertension and SMM than the overall population. This is consistent with other research findings related to disparate health outcomes for non-white patients.
Figure 3. Rates of Hypertension, Hemorrhage, and Severe Maternal Morbidity (SMM), Overall and by Race
Health disparities such as these are an area of focus within the MVC Coordinating Center’s broader strategic framework. MVC’s health equity sub-committee meets regularly to strategize how to emphasize equity among its membership and support related quality improvement initiatives. The Coordinating Center’s aim is to use MVC data to help members identify areas of opportunity and support quality improvement through collaboration with peers. To this end, MVC is currently developing a hospital-level adaptation of the new statewide birth outcomes report to share site-specific data with its members later this year.
“Claims data such as those included in MVC’s episodes of care present a great opportunity to use state-wide data to highlight important findings and disparities related to birth outcomes in Michigan,” said Kristen Hassett, the lead MVC analyst for the analysis. “This report represents an important step in MVC’s work to identify areas of health inequality and then support initiatives to reduce those disparities.”
For the MHA Keystone Center, the statewide report provides valuable data to further inform its work.
“We are proud to partner with organizations like the Michigan Value Collaborative to collect and examine critical data related to childbirth within Michigan health systems,” said Sarah Scranton, vice president of safety and quality at MHA and executive director of MHA Keystone Center. “By evaluating hemorrhage, hypertension and severe maternal morbidity rates across several regions of the state, we are able to address the challenges facing Michigan mothers and birthing centers.”
The MVC statewide childbirth episodes report will aid MHA’s field engagement team while they engage with hospitals not yet partnering with MI AIM. Since its adoption in Michigan in 2016, MI AIM has contributed to significant improvement in hemorrhage-related SMM, hypertension-related SMM, and overall SMM through the implementation of hemorrhage, hypertension, and sepsis patient safety bundles with Michigan birthing hospitals.
To view the complete report, visit the MVC website. The Coordinating Center welcomes any additional questions about the report findings or any custom report analyses inspired by its creation. Contact the MVC team at Michigan-Value-Collaborative@med.umich.edu.
