For the last two years, the Michigan Value Collaborative (MVC) Coordinating Center has offered a sepsis service line developed in partnership with the Michigan Hospital Medicine Safety Consortium (HMS). In conjunction with this work, reports customized to each member hospital are distributed each year. The most recent iteration shared with members this week features several updates from the 2021 versions.
A new patient population snapshot table is one new feature that the MVC Coordinating Center added in order to integrate its demographic data. These tables (see Figure 1 for a sample table of a blinded acute-care hospital) provide each hospital with demographics for their sepsis patient population, including race, mean age, top patient zip codes, the most frequent and average number of comorbidities, the proportion of dual-eligible patients, and the proportion of patients with a confirmed diagnosis of COVID-19. Furthermore, this data is stratified by payer, providing additional insights into specific groups of patients.
Figure 1.
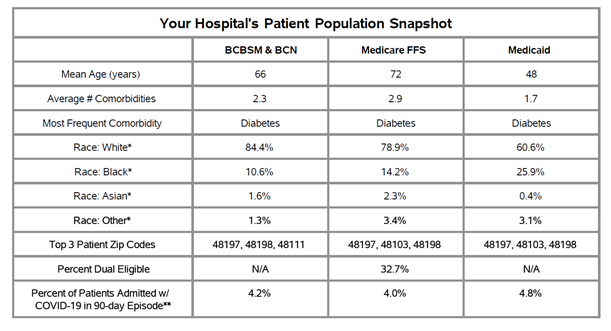
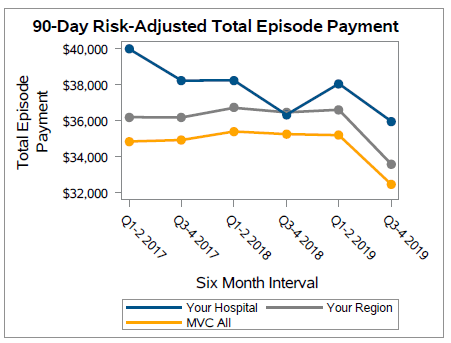
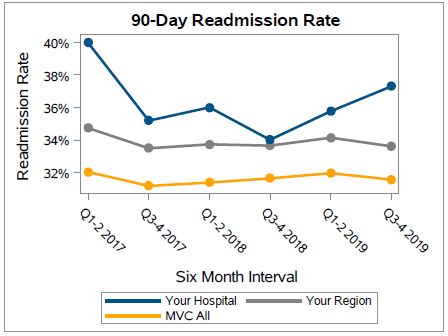
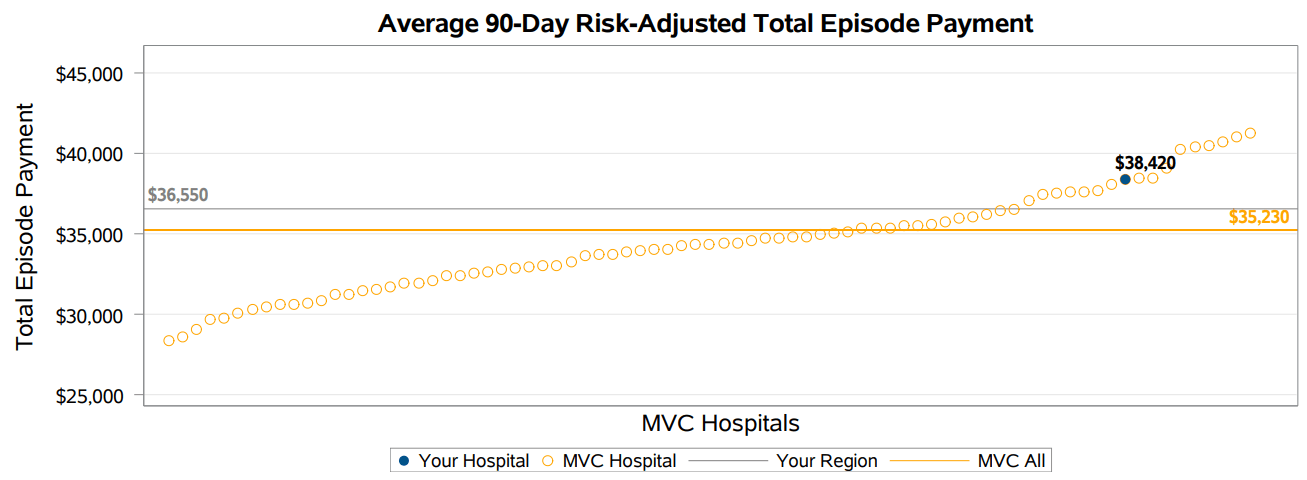
The inclusion of COVID-positive patient percentages is an important statistic since this iteration of the sepsis push report includes COVID patients, whereas the Coordinating Center removed these patients in previous versions. This final row of the patient population snapshot table will help hospitals understand the extent to which their data is driven (or not) by patients with a confirmed COVID diagnosis code. Across the collaborative, 90-day total episode payments increased in 2020, which can likely be attributed to episodes with a COVID diagnosis; however, the 2020 average is not much higher than the average from 2018 through early 2019 (see Figure 2). Since the COVID-19 pandemic hit regions of Michigan at different times, regional comparisons for select measures will be particularly useful in understanding one’s data. Different versions of the report were created for acute-care and critical access hospitals, which allowed for tailored comparison groups.
Figure 2.
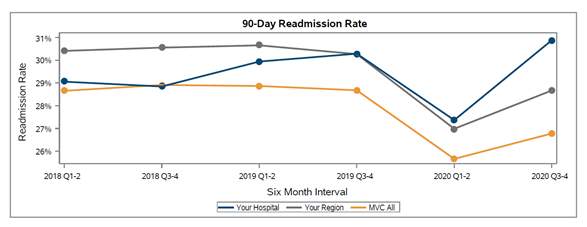
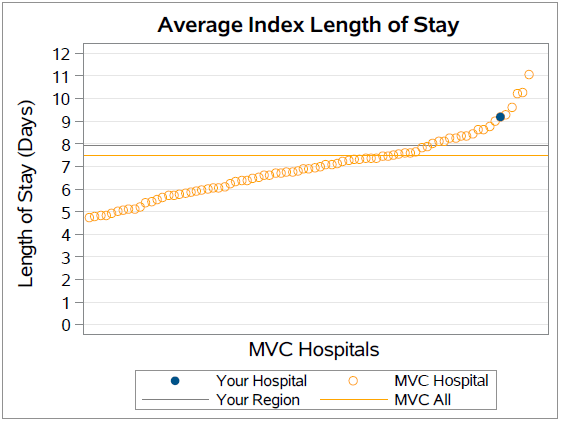
The complete report compares MVC hospitals on 90-day risk-adjusted total episode payments, inpatient length of stay, Intensive Care Unit (ICU)/Cardiac Care Unit (CCU) utilization, inpatient mortality and discharge to hospice, 90-day post-acute care utilization, and 90-day readmission rates. Each figure presented reflects index admissions from 1/1/18 – 12/31/20 for Medicare FFS, Blue Cross Blue Shield of Michigan (BCBSM) PPO Commercial, Blue Care Network (BCN) Commercial, BCBSM PPO Medicare Advantage, BCN Medicare Advantage, and Medicaid.
In addition to continuing to offer its sepsis push reports, the MVC Coordinating Center also offers a bimonthly sepsis workgroup. The next workgroup will take place on Thursday, May 26 from 2-3 p.m., and will feature a presentation about successes in sepsis-bundle compliance. Register today to join the MVC Coordinating Center for this presentation and discussion.
If you have any suggestions on how these reports can be improved or the data made more actionable, the Coordinating Center would love to hear from you. We are also seeking feedback on how collaborative members are using this information in their quality improvement projects. Please reach out at michiganvaluecollaborative@gmail.com.