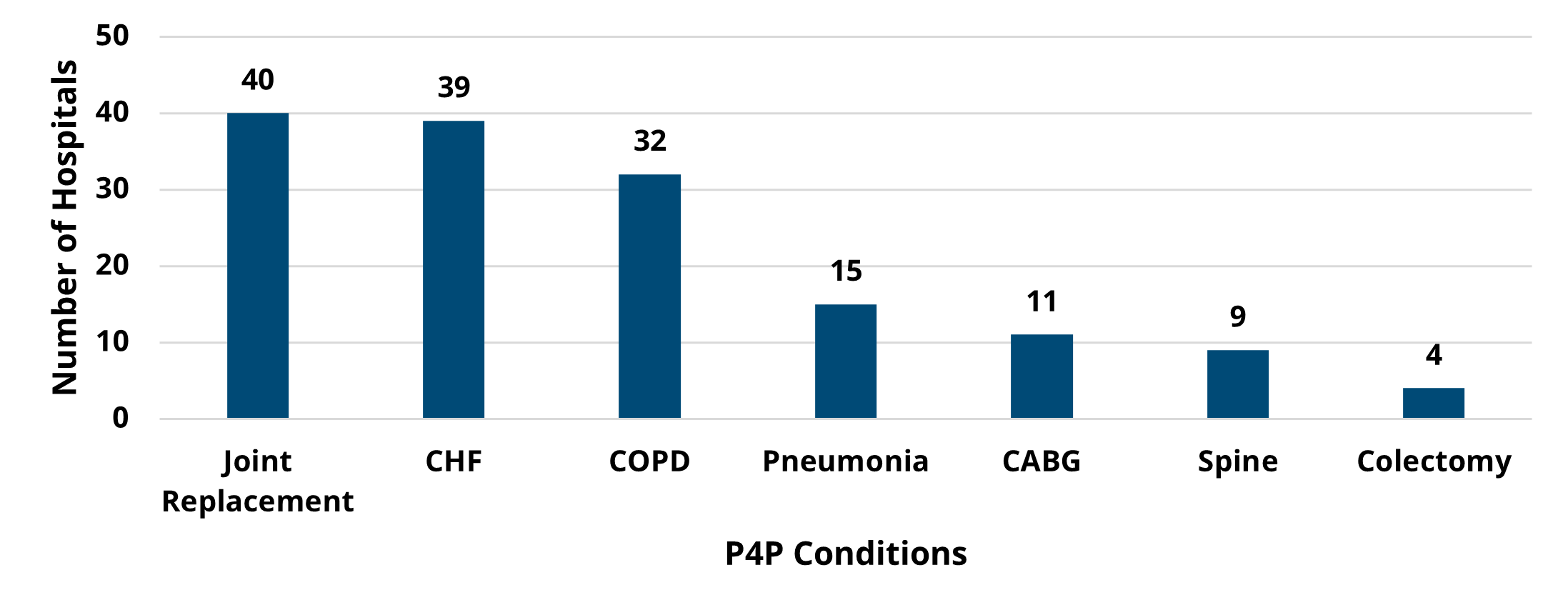
The Michigan Value Collaborative (MVC) Coordinating Center distributed a new report earlier this month focused on Program Years (PYs) 2024 and 2025 for the MVC Component of the Blue Cross Blue Shield of Michigan (BCBSM) Pay-for-Performance (P4P) Program. PYs 2024 and 2025 retained the episode spending component of the program but incorporated MVC’s value metrics – specific process measures of utilization that are evidence-based, actionable, and show variability across the state. This report, therefore, highlighted data for each hospital’s specific PY 24-25 episode spending and value metric selections. We hope that these reports will be utilized to inform quality improvement efforts by identifying areas of opportunity for episode spending conditions or value-based practices.
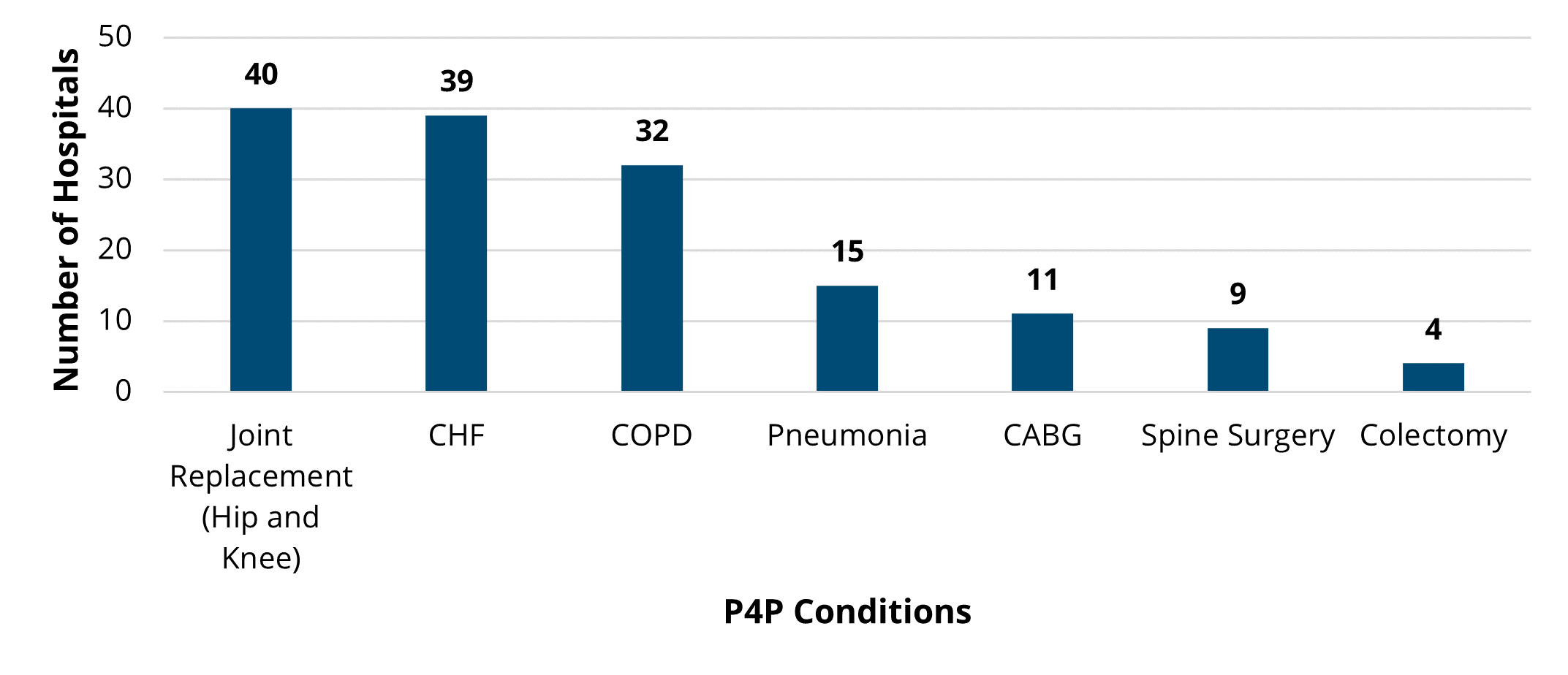
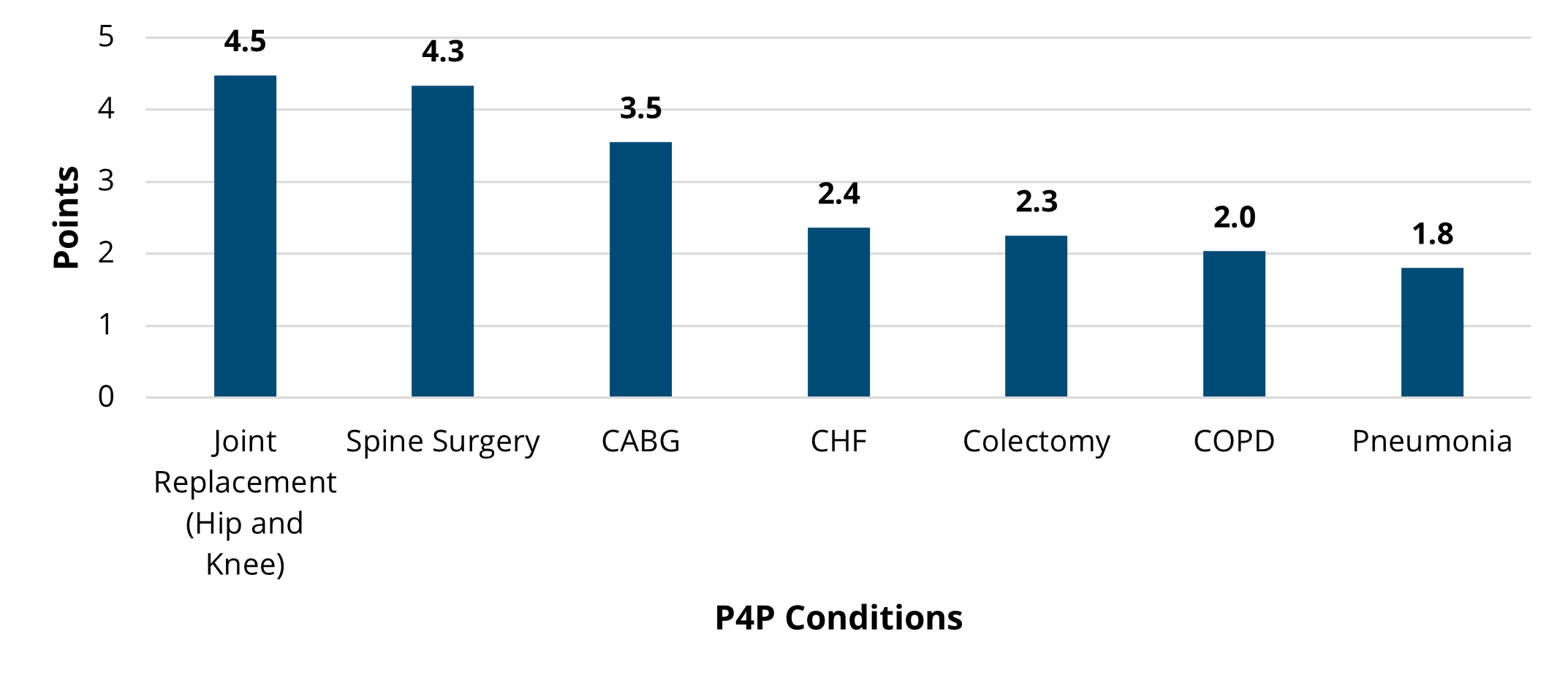
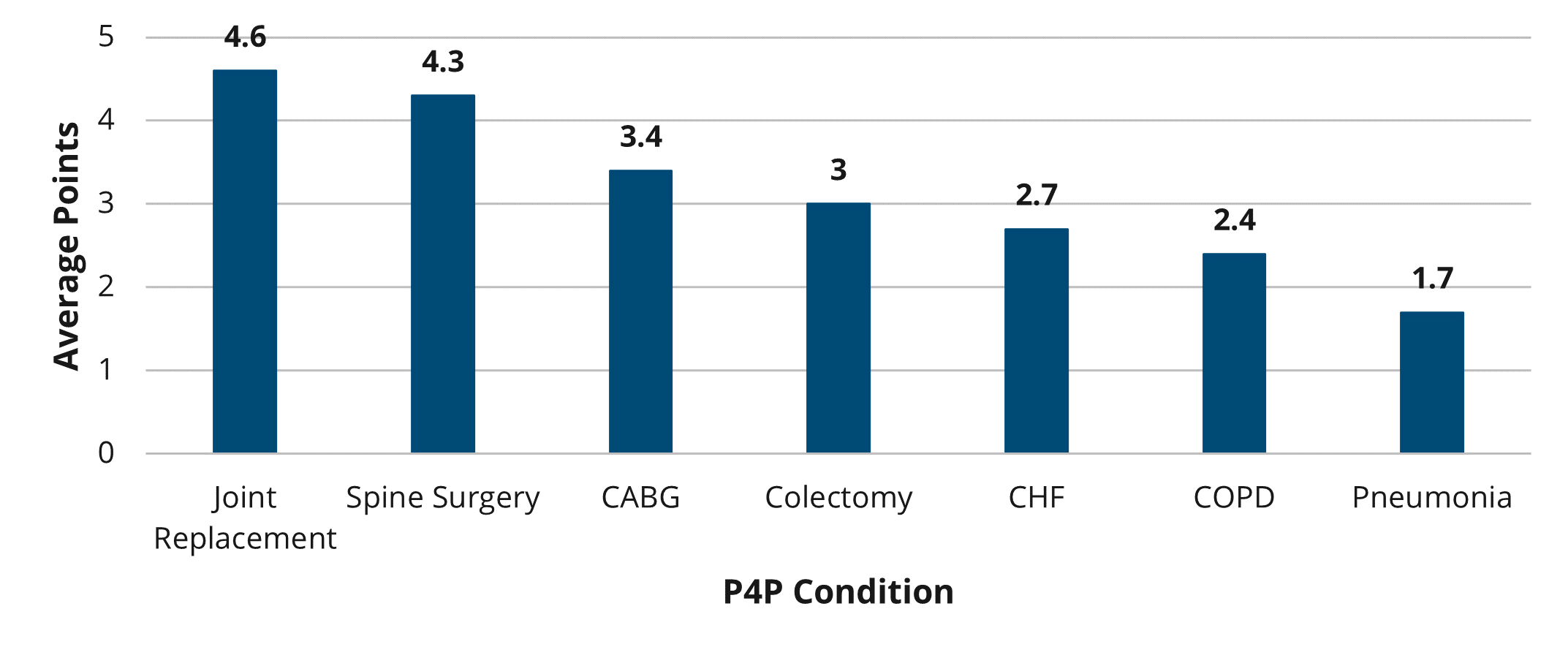
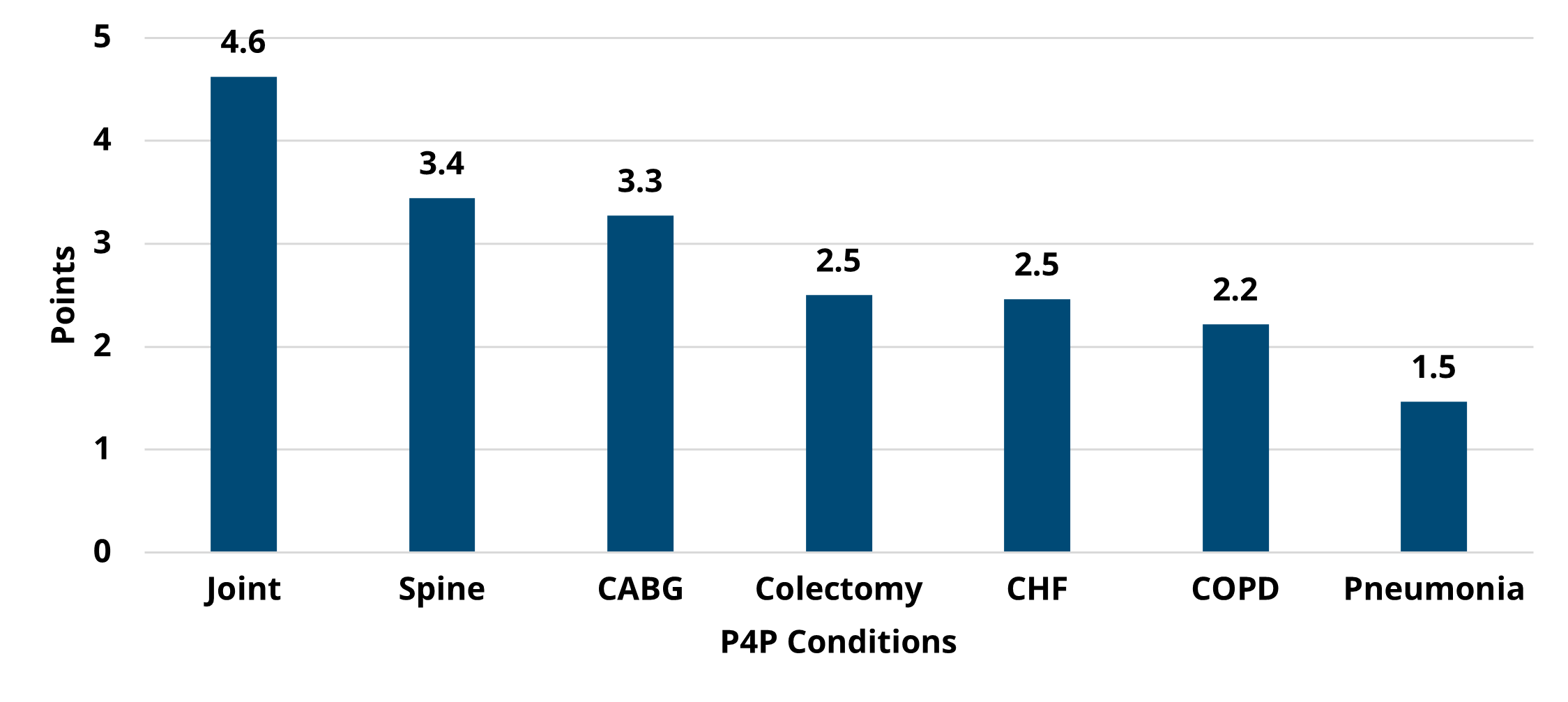
Hospitals selected chronic obstructive pulmonary disease (COPD), colectomy (non-cancer), congestive heart failure (CHF), coronary artery bypass grafting (CABG), joint replacement, or pneumonia for their episode spending scoring. Seven value metrics were available to choose from, including cardiac rehabilitation after CABG, cardiac rehabilitation after percutaneous coronary intervention (PCI), seven-day follow-up after CHF, 14-day follow-up after COPD, seven-day follow-up after pneumonia, preoperative testing, and risk-adjusted readmission after sepsis. With the exception of the trend figure on the report’s value metric page (which has a data range of 1/1/2020 – 12/31/2022), the data in this report reflected baseline year data (2021) for PY 2024. Any impact to utilization or patient outcomes achieved by hospitals this year will contribute to their performance year data for PY 2025.
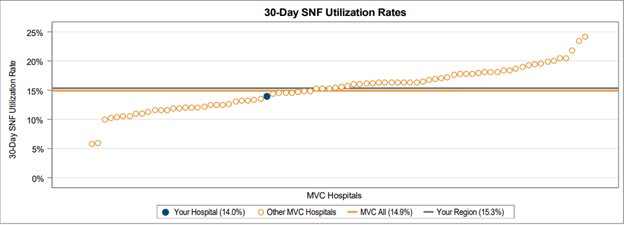
The first data page focused on a hospital’s episode spending selection, and provided a caterpillar plot (Figure 1) for price-standardized and risk-adjusted total episode payments for that hospital compared to other MVC hospitals as well as the MVC collaborative-wide average and that hospital’s P4P cohort average. P4P cohorts were determined based on hospital bed size, case mix index, and critical access status.
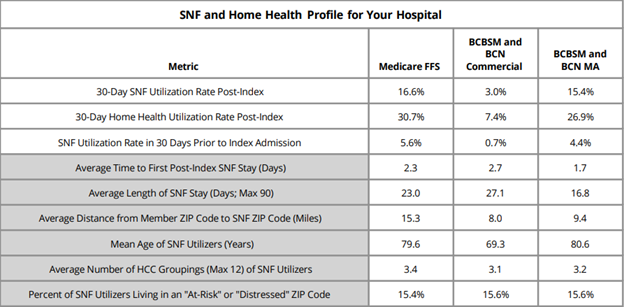
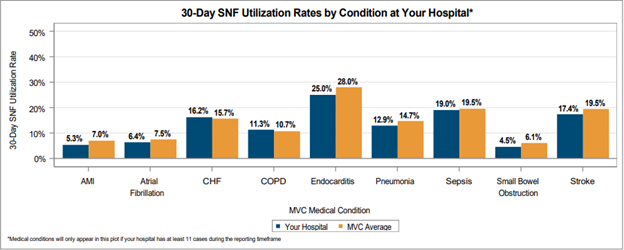
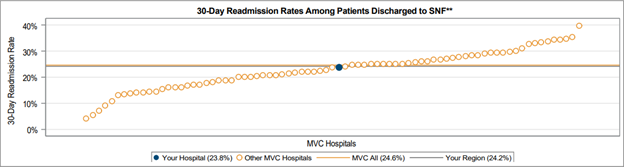
The report also included episode spending figures focused on price-standardized, risk-adjusted payments for major episode components (index, professional, readmission, and post-discharge) as well as post-discharge payment components (emergency department, home health, skilled nursing facility, inpatient and outpatient rehab, and outpatient services). These two figures (Figure 2 and 3) could be used to identify the components contributing most significantly towards a hospital’s total episode payment.
The second data page provided information about a hospital’s value metric selection. The first figure was a caterpillar plot (Figure 4) displaying that hospital’s value metric rate compared to other MVC hospitals as well as the MVC collaborative-wide average and that hospital’s P4P cohort average.
The value metric page also included a trend graph detailing a hospital’s value metric rate by six-month interval, and a final figure that varied by hospital to provide additional metric-specific insights. Hospitals being scored on cardiac rehab after CABG or PCI received a caterpillar plot of average days to the first cardiac rehab visit among cardiac rehab utilizers. Hospitals being scored on follow-up after CHF, COPD, or pneumonia received a bar chart of follow-up rates by setting (in-person only, remote only, or both in-person and remote). Hospitals being scored on preoperative testing will see a bar chart of preoperative testing rates by test type. Lastly, hospitals being scored on 30-day readmissions after sepsis received a table of the most common reasons for readmission after the initial sepsis episode’s discharge.
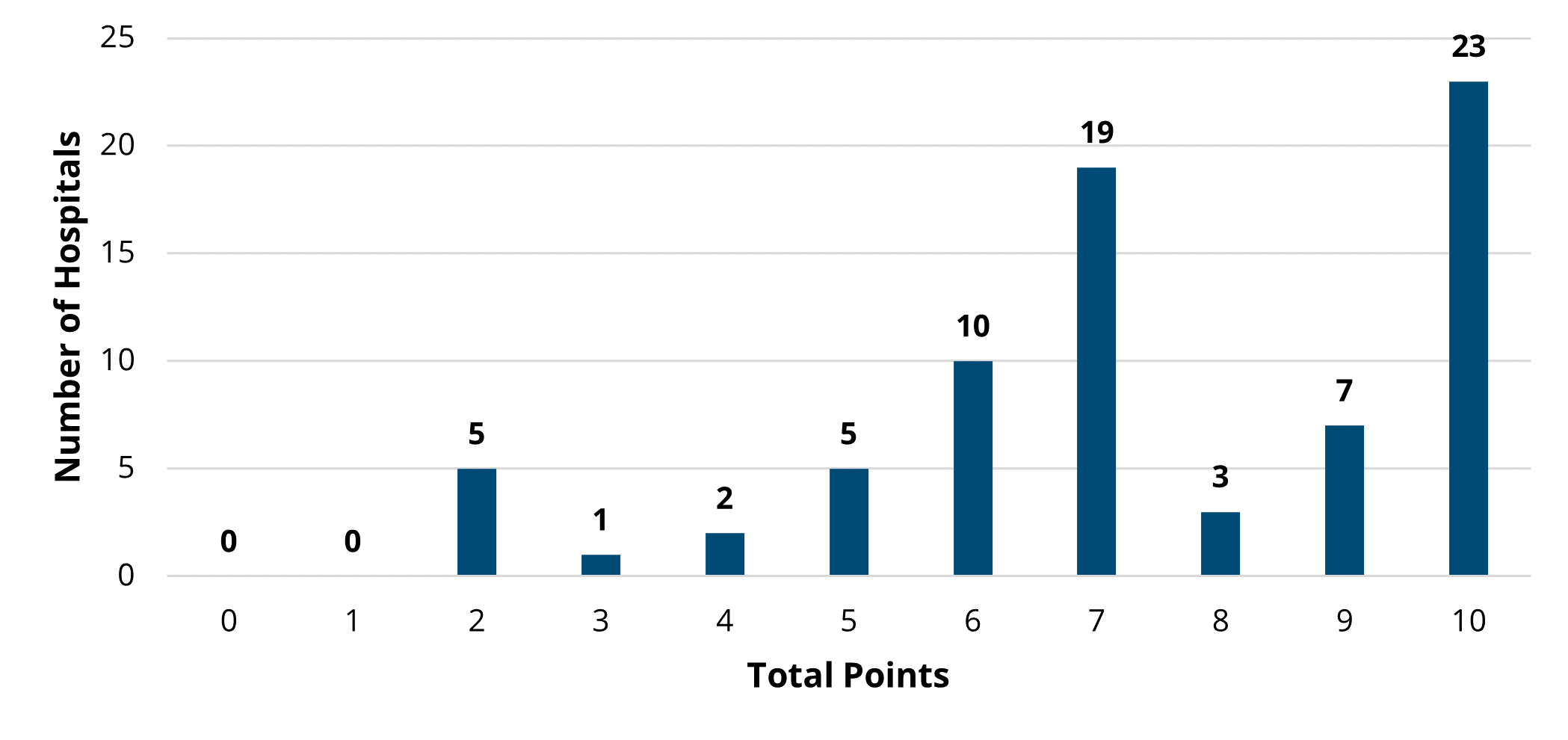
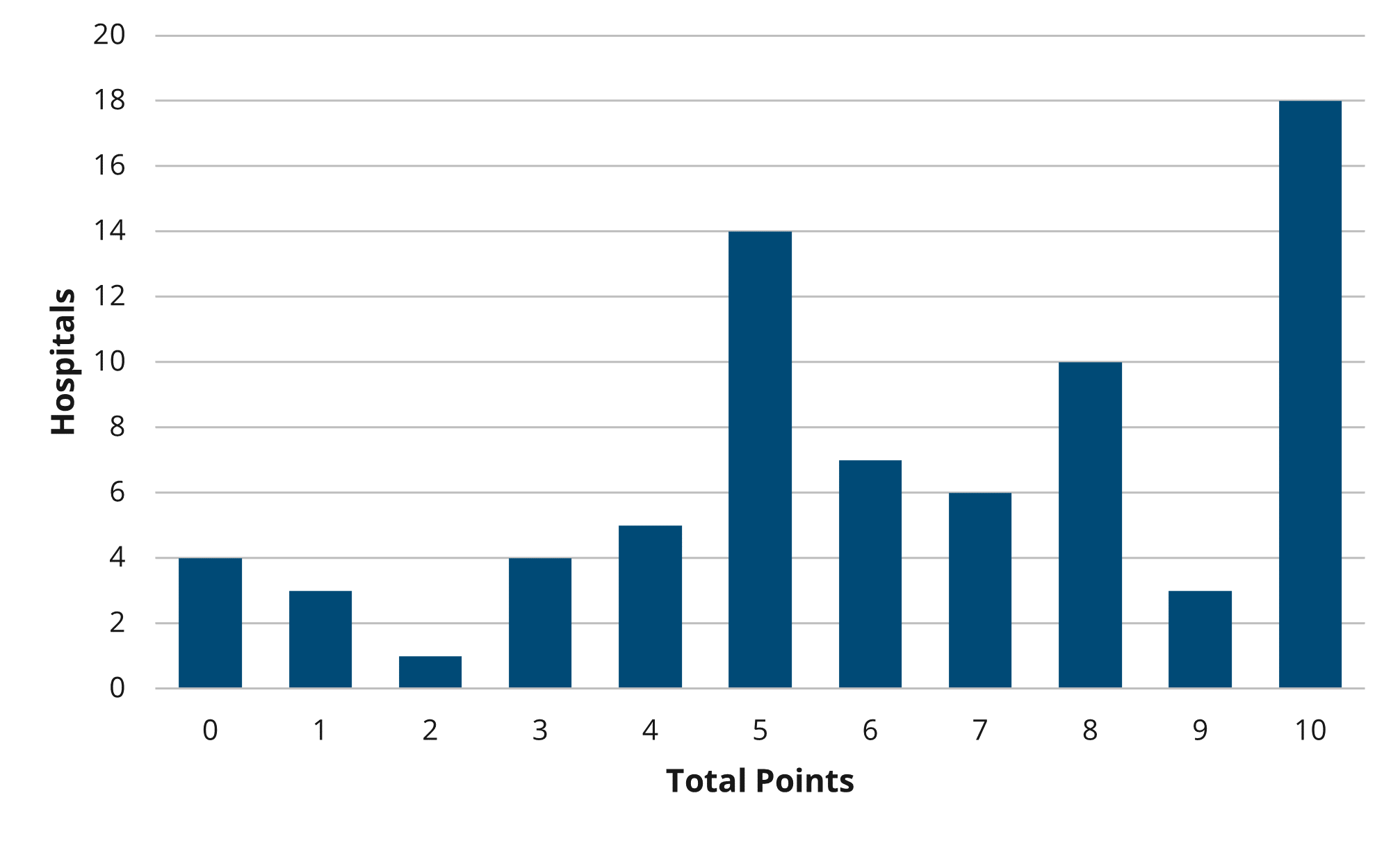
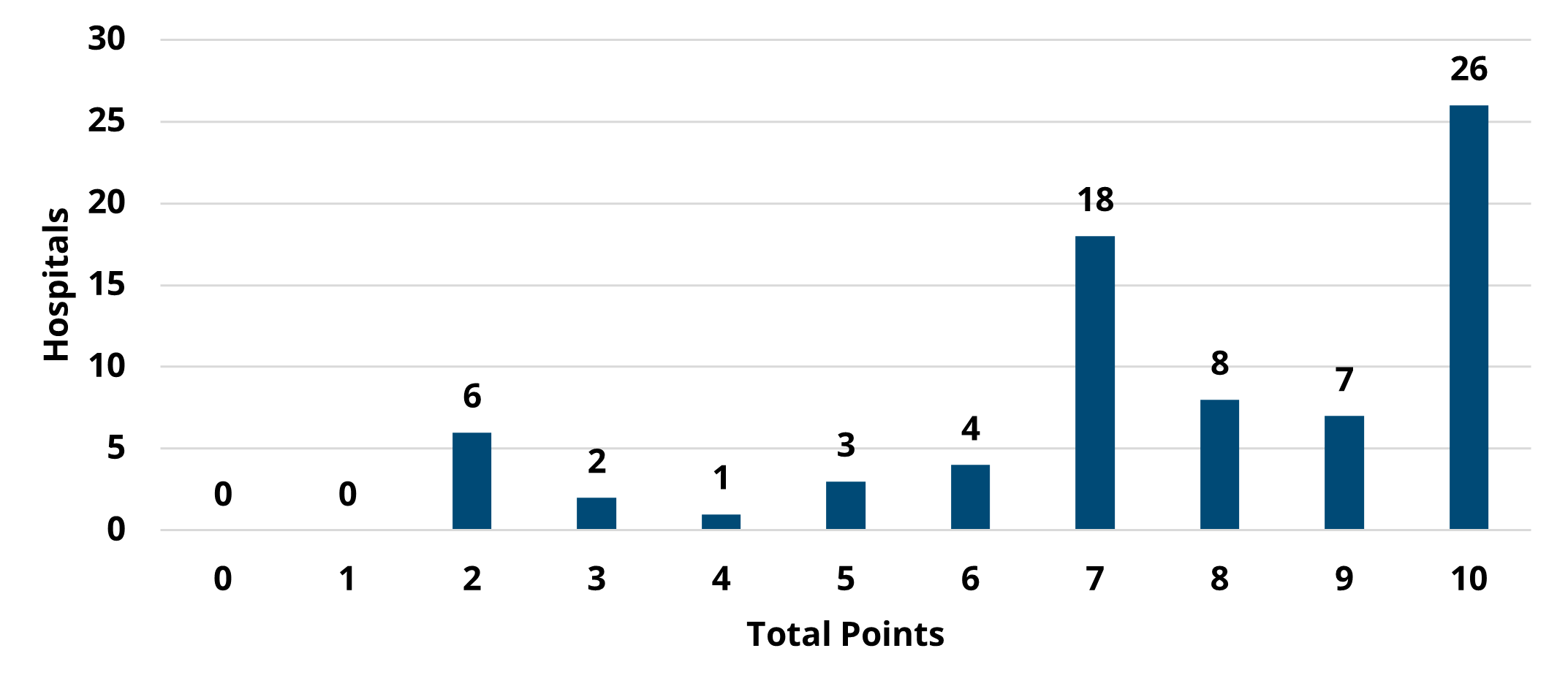
For more information about your hospital’s episode spending and value metric selections and data, as well as other conditions and value metrics not selected, hospitals can utilize the PY 2024-2025 reports on the MVC Registry. PYs 2024 and 2025 also introduced a new engagement component, awarding 2 out of the 10 program year points for completed engagement activities. Please see the following event list and calendar for 2024 engagement opportunities, which will contribute to a hospital’s PY 2024 score.
If you have any questions regarding the MVC Component of the BCBSM P4P Program, please reference the P4P Technical Document for Program Years 2024 and 2025. If you would like to set up a meeting to review your hospital’s performance, please contact the Coordinating Center at Michigan-Value-Collaborative@med.umich.edu.