This week MVC distributed its second preoperative testing push report of 2022, providing members with another opportunity to benchmark their testing practices. MVC first introduced its preoperative testing push reports in 2021 to help members reduce the use of unnecessary testing for surgical procedures. Preoperative testing, especially for low-risk surgeries, often provides no clinical benefits to patients but is ordered regularly at hospitals across Michigan.
The report distributed this week had many similarities to the version distributed earlier this year in April, namely that members continued to see their rates across a variety of tests for three elective, low-risk procedures performed in outpatient settings: laparoscopic cholecystectomy, laparoscopic inguinal hernia repair, and lumpectomy. Claims were evaluated for the index event as well as 30 days prior to the procedures for the following common tests: electrocardiogram (ECGs), echocardiogram, cardiac stress test, complete blood count, basic metabolic panel, coagulation studies, urinalysis, chest x-ray, and pulmonary function.
The latest report has a few key differences from the spring version, the most significant of which is that it utilizes claims from Blue Cross Blue Shield of Michigan (BCBSM) and Blue Care Network (BCN) plans exclusively. This allows members to see MVC’s most up-to-date data; the report includes index admissions from 1/1/2019 through 12/31/2021. In addition, since the report contains BCBSM/BCN data only, there is no case count suppression, whereas members would only see their data in the spring version if they had at least 11 cases in each year of data for the three combined conditions.
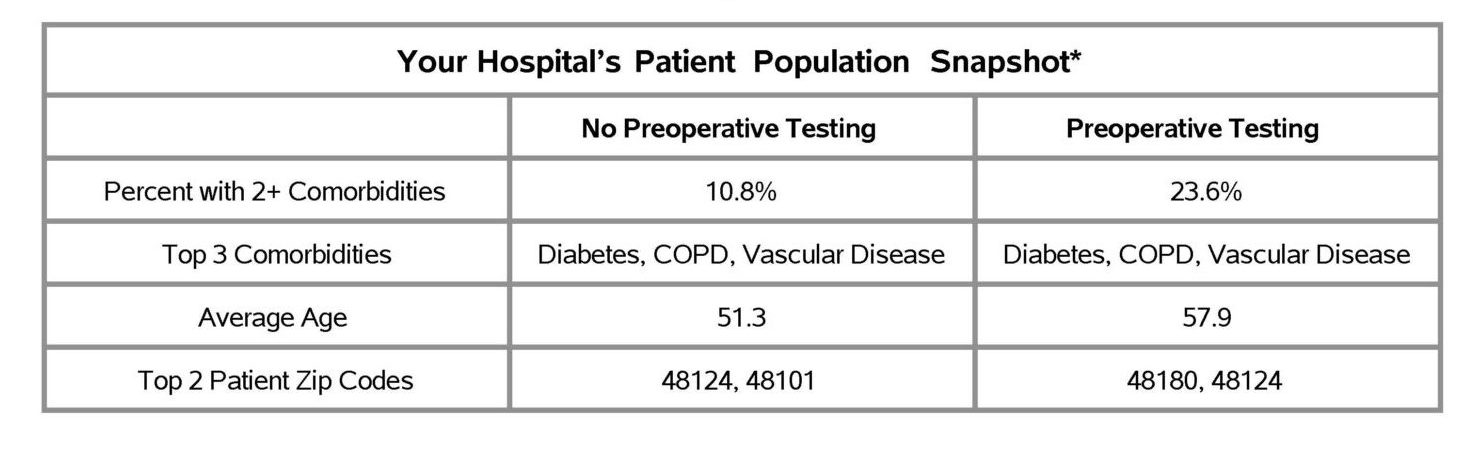
The reports received by members this week included several new figures. Similar to other MVC push reports, members will now see a patient snapshot table that provides additional information about the report’s patient population. For this, MVC chose to include patient characteristics such as age, zip code, and comorbidities. Generally speaking, there were more comorbidities among patients who underwent preoperative testing compared to patients with one or no comorbidities (see Figure 1). However, the majority of patients who complete a preoperative test do not have multiple comorbidities. There were also observed differences in testing rates by age. In general, patients who had preoperative testing were older on average than patients who had no preoperative testing.
Figure 1.
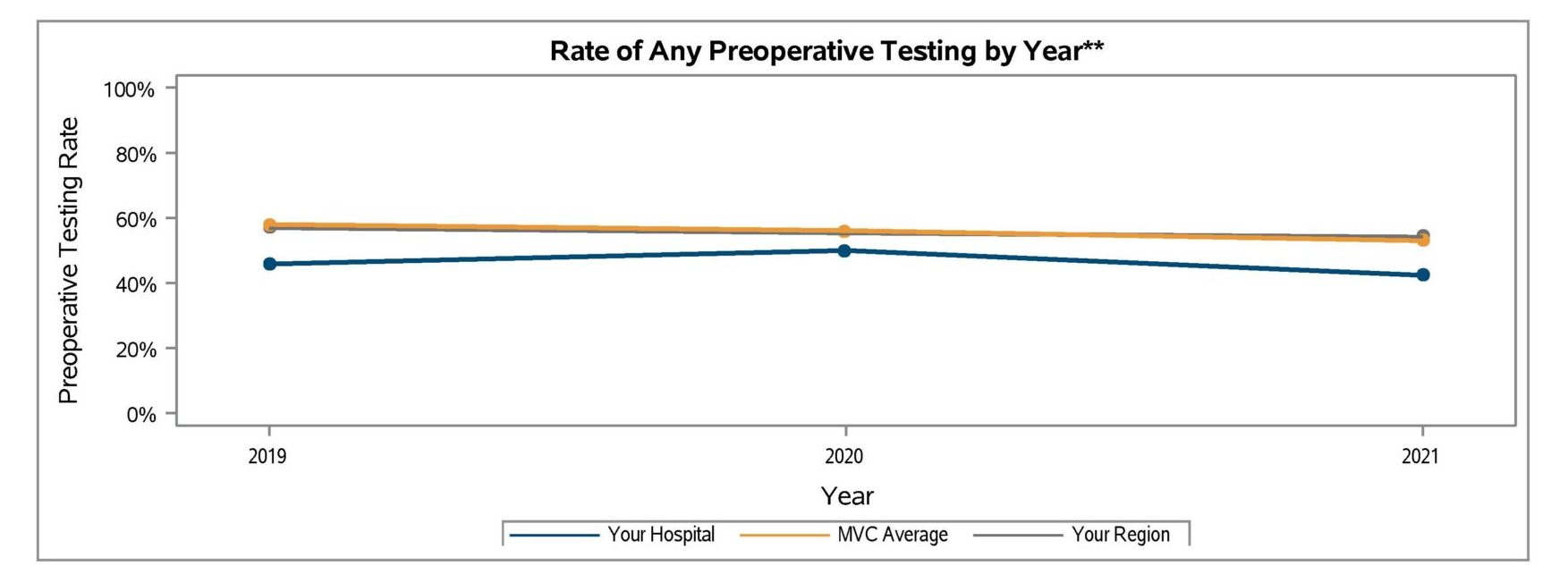
Another new figure showcased the overall preoperative testing rates by year. This trend graph showed members how their overall rate for any preoperative testing compared in 2019, 2020, and 2021, and it included data points for the MVC average and regional comparison groups (see Figure 2). The key finding for this figure was that there has been very little change in testing rates over time when looking at overall preoperative testing practices. This means that, in general, the prevalence of low-value preoperative testing has remained consistently high overall across the collaborative for three years and likely longer.
Figure 2.
The latest report also included a new figure for absolute change in any preoperative testing from 2019 to 2021. For each hospital, this appears as a caterpillar plot of absolute change percentages for their highest-volume procedure among the three low-risk surgeries in the report. Members can see the percentage change—positive or negative—in their testing rate for that surgical condition, as well as how their absolute change compares to the rest of the collaborative. For example, hospitals that perform more cholecystectomies than hernia repairs or lumpectomies saw a wide range of both increases and decreases in preoperative testing rates from 2019 to 2021 (see Figure 3).
Figure 3.
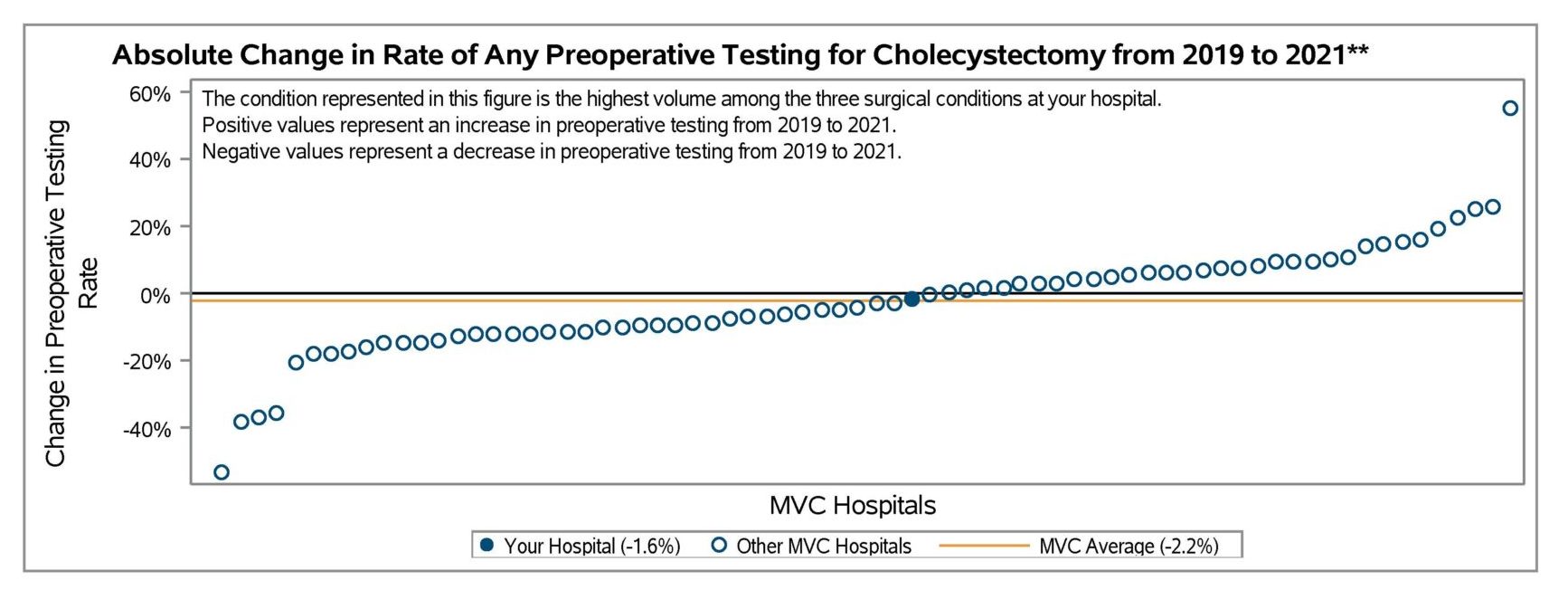
The blinded hospital in this example observed very little change in its testing rate for cholecystectomy (-1.6%), and the MVC average was similar (-2.2%). This showcases that although the collaborative is not seeing much change to overall rates for any testing over time, individual members might see greater variability over time for specific tests or procedures, especially in instances of low case counts.
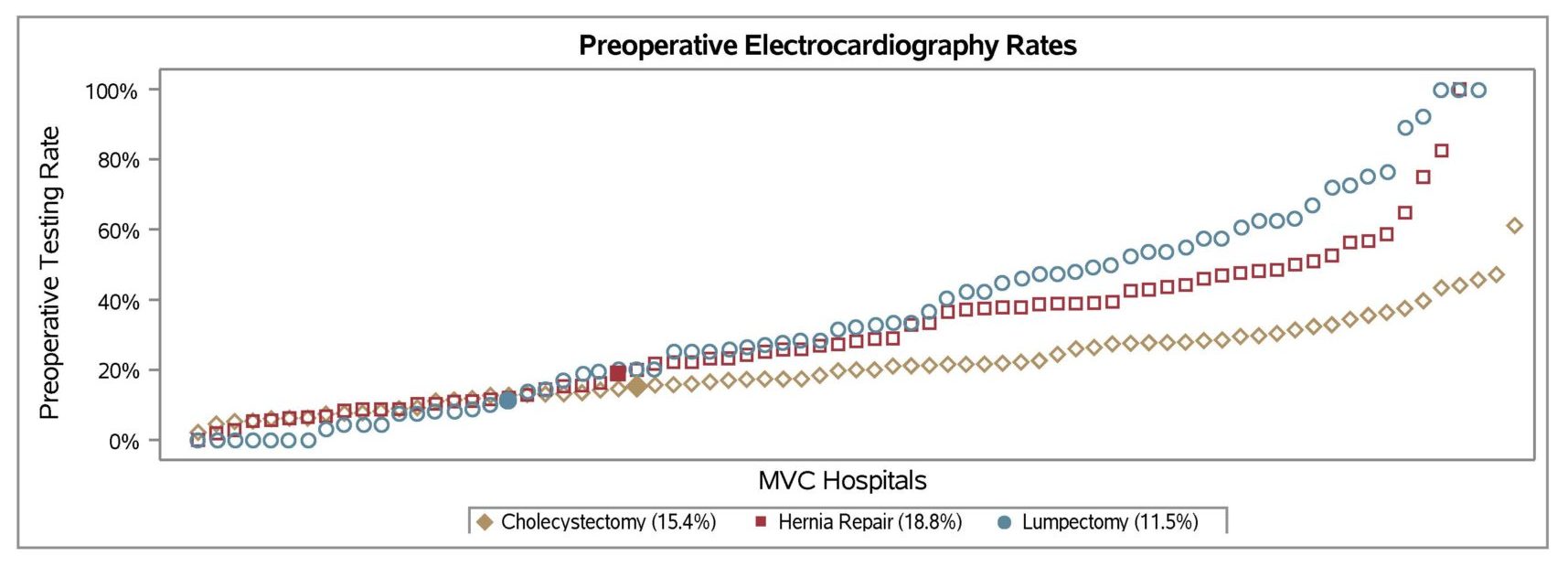
Members will be able to take those deeper dives into their rates for specific tests in the figures that make up the remaining pages of the report. Viewing one’s preoperative testing rates for each specific test can help members understand if any specific tests are driving their overall testing rate. One area of opportunity, for example, could be to reduce one's rate of cardiac testing, specifically ECGs; the rate of ECGs is very variable across the collaborative (see Figure 4) and could lead to a cascade of care.
Figure 4.
MVC is eager to drive improvement in this area. For more information on how MVC is working to reduce unnecessary preoperative testing, visit its Value Coalition Campaign webpage here. If you are interested in a more customized report or would like information about MVC’s preop testing stakeholder working group, please contact the MVC Coordinating Center at michiganvaluecollaborative@gmail.com.




