This month MVC hosted its first post-discharge follow-up workgroup presentation of the year, which featured a presentation by guest speaker Lisa Powell, MBA, PTA, Clinical Director of Operations of Sparrow Hospital. She shared insights from a recent Sparrow Hospital project launched to reduce readmissions and acute care utilization.
The project came about when E.W. Sparrow Hospital identified that readmissions were a key driver of capacity limitations in the acute care setting and that Sparrow was underperforming compared to peers. After observing high readmission rates for their facility, Sparrow investigated utilization by asking questions about the social determinants of health impacting the patient population and looking into specific identity metrics.
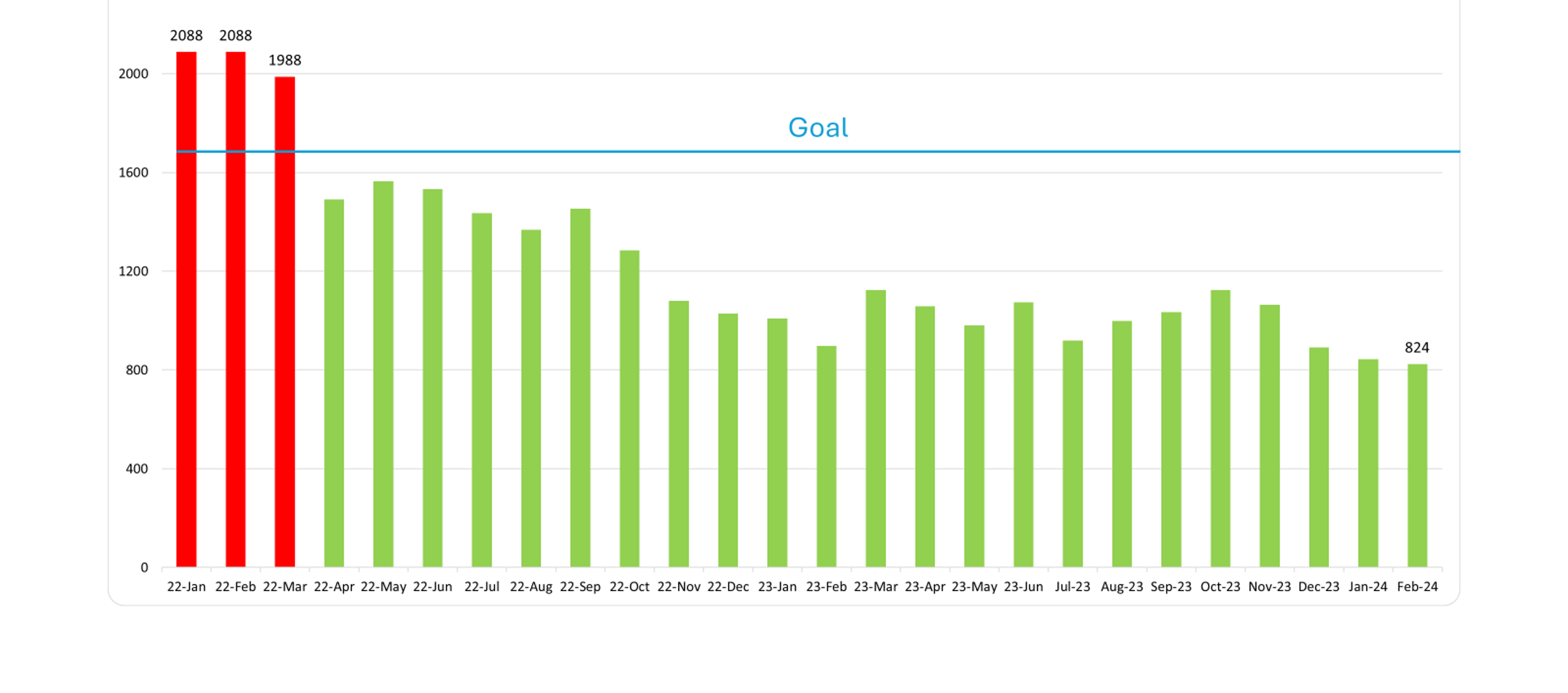
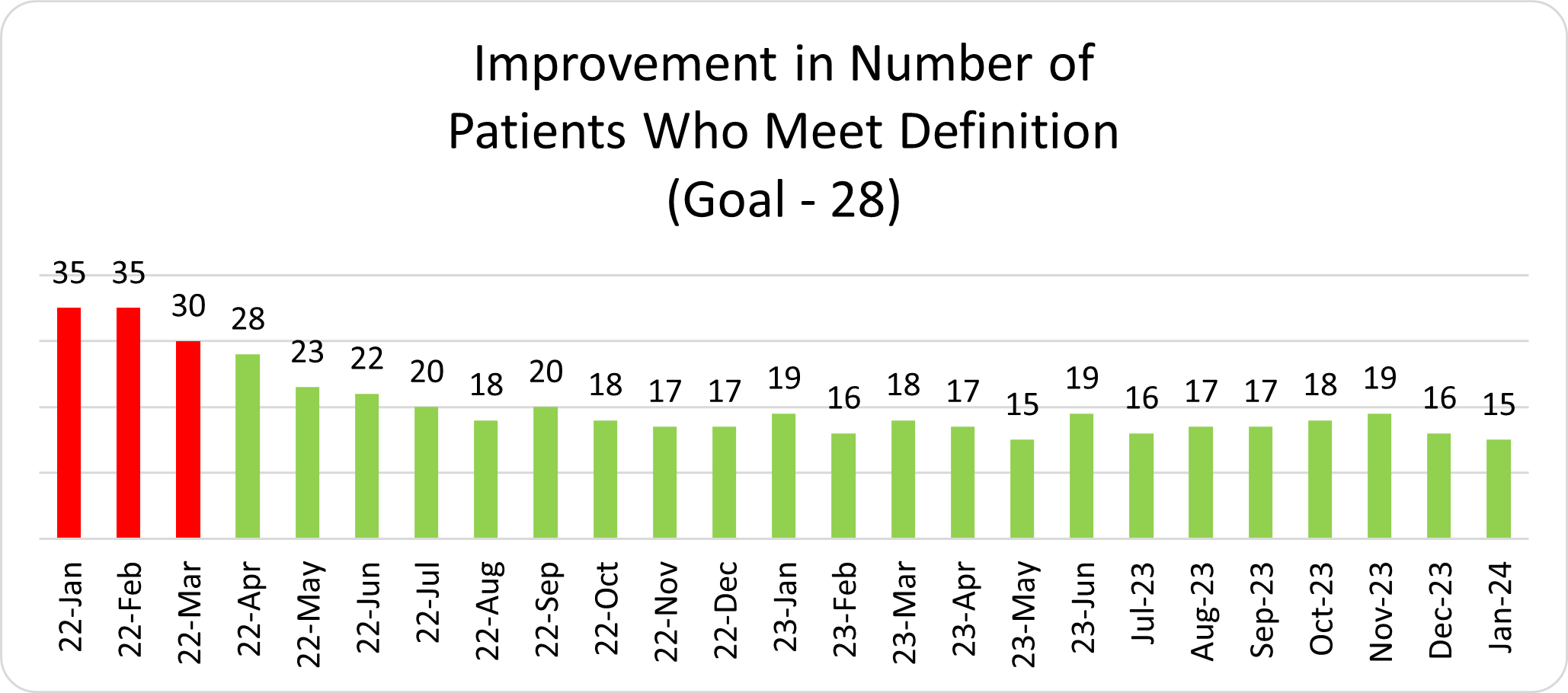
As part of Sparrow’s investigation, they drilled down on specific patient cases for context, discovering 35 discrete patients in 2021 who accounted for a total of 434 admissions and 2,088 acute care days. This unique subset of patients was defined by the Sparrow team as multiple-visit patients (MVPs)—those with 10 or more combined inpatient and observation admissions over the past 12 months. The data available on MVPs exemplified a disconnect in the delivery, management, and transition of care, and a need for a care plan that could be implemented the next time an MVP patient presented to the emergency department. The resulting plan was designed to transition away from episodic care, close the primary care gap to improve care in the right setting, and remove barriers to accessing specialty care, all within Sparrow's resource and time constraints.
Focusing on one patient at a time, the physicians and care team members were tasked to work offline on their own time to articulate a brief care plan and synopsis of the patient from their respective disciplines. The providers later came together at one-hour multidisciplinary virtual meetings to discuss each patient and achieve consensus on their proposed plan. Once a plan was established and agreed upon, the team distributed the information to hospital staff utilizing layered EMR tools such as FYI flags, specialized note types for MVP care plans, and best practice advisories (BPA).
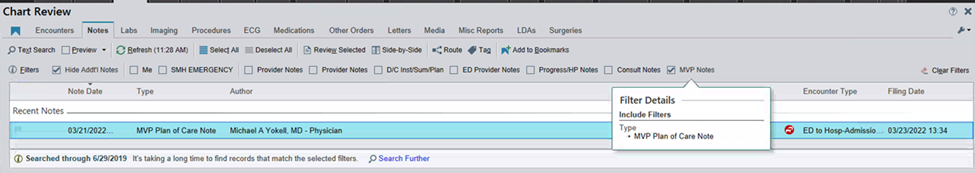
After receiving initial feedback and analyzing usage data, providers found certain EMR tools more effective than others. FYI flags were the least utilized tool and not effective on their own in changing clinical behavior, as they were often ignored. Implementing a specialized note type for MVP care plans, however, was extremely effective and user-friendly (Figure 2). Through this development, providers no longer needed to search through lengthy patient medical histories to locate their MVP care plan, increasing the likelihood that the care provided would be in line with the agreed upon multidisciplinary plan.
Four months after Sparrow Hospital launched this EMR systems approach, they reduced acute care days as well as the number of patients who met the multi-visit patient definition of 10 or more admissions over 12 months (see Figures 3 and 4) with sustained improvement for over two years. Providers consistently provide positive feedback and Sparrow has continued to expand the scope and use of the approach.
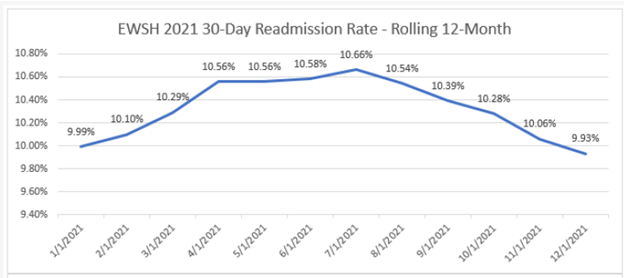
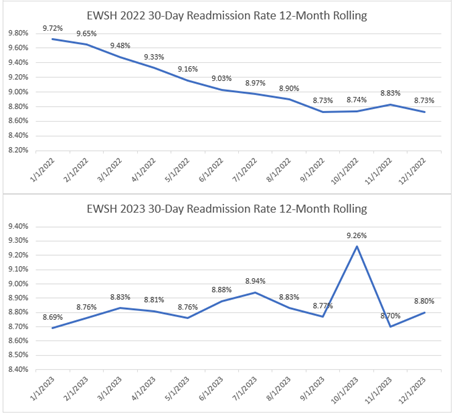
Although over the past two years, readmission rates and the number of MVPs that frequent their hospital have decreased (Figure 5), the impact of this project expands far beyond improving hospital readmission rates and acute care utilization. Sparrow Hospital’s systems approach to MVPs keeps patients out of the hospital and improves their lives. Although no patient-reported outcomes data has been collected on this to date, Sparrow Hospital is confident that this approach is improving the quality of life for many patients.
As the project continues to evolve, Sparrow Hospital hopes to expand the utilization of multidisciplinary care plans delivered through EMR tools, which are inherently designed for flexibility in use. The target population can be broadened, providers can escalate patients who may benefit from an MVP plan of care, and tools can be utilized for difficult transitions of care.
Sparrow’s systems-level approach to supporting MVPs in a hospital setting has shown great promise in care management and improvement, and the participants in last week’s workgroup were eager to share the success of this project with their sites and colleagues. Sparrow Hospital identified an area of poor performance and collaborated to design an initiative that addressed patient needs within established systems and resources. As we look toward the future of healthcare quality improvement, feasibility in implementation must be a high priority to achieve success.
MVC workgroups consist of a diverse group of representatives from Michigan hospitals and physician organizations that meet virtually to collaborate and share ideas. If you were unable to attend this workgroup, you can access the recording here. To register for upcoming workgroups, visit MVC’s 2024 events calendar. If your team has a successful initiative or project to share with the Collaborative, please reach out to MVC.