The Michigan Value Collaborative introduced its first colectomy physician organization (PO) report this week. A colectomy is the surgical removal of a section of the large intestine (colon) or bowel and is performed to treat diseases of the bowel (i.e., Crohn’s disease, ulcerative colitis, and colon cancer).
The report incorporated administrative claims of attributed members from 1/1/19 – 12/31/20 for Blue Cross Blue Shield of Michigan (BCBSM) PPO Commercial and BCBSM Medicare Advantage, and 1/1/19 – 9/30/20 for Medicare Fee-for-Service. Reports were created for all POs that currently participate in MVC and had at least 11 colectomies per year in both 2019 and 2020.
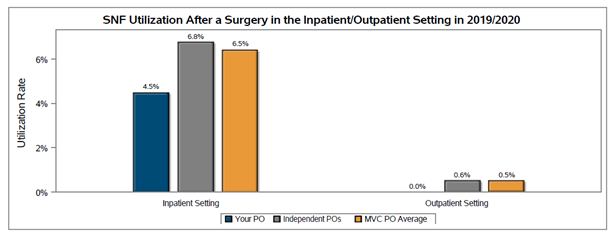
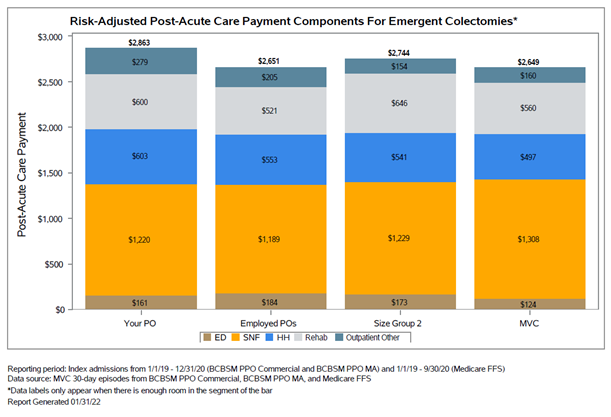
There were significant differences in the anticipated clinical course and the likelihood of complications between elective (planned) and emergent colectomy. Therefore, MVC provided a stratified summary of planned versus emergent colectomies (Figure 1), and some metrics in the report were stratified by planned and emergent status to highlight when there was an emergency department revenue code on the episode. For example, there were notable differences in post-acute care utilization between planned and emergent colectomies (Figures 2 & 3).
Figure 1. PO A Colectomy Report Table
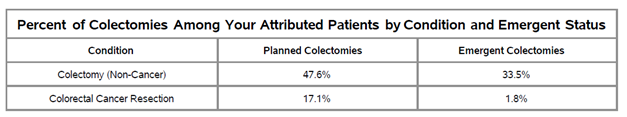
Figure 2. PO A Risk-Adjusted Payments: Planned Colectomies
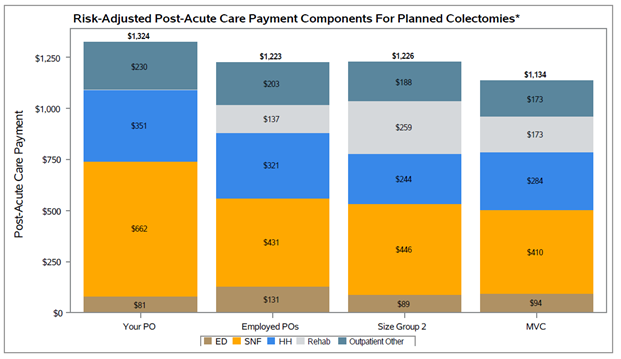
Figure 3. PO A Risk-Adjusted Payments: Emergent Colectomies
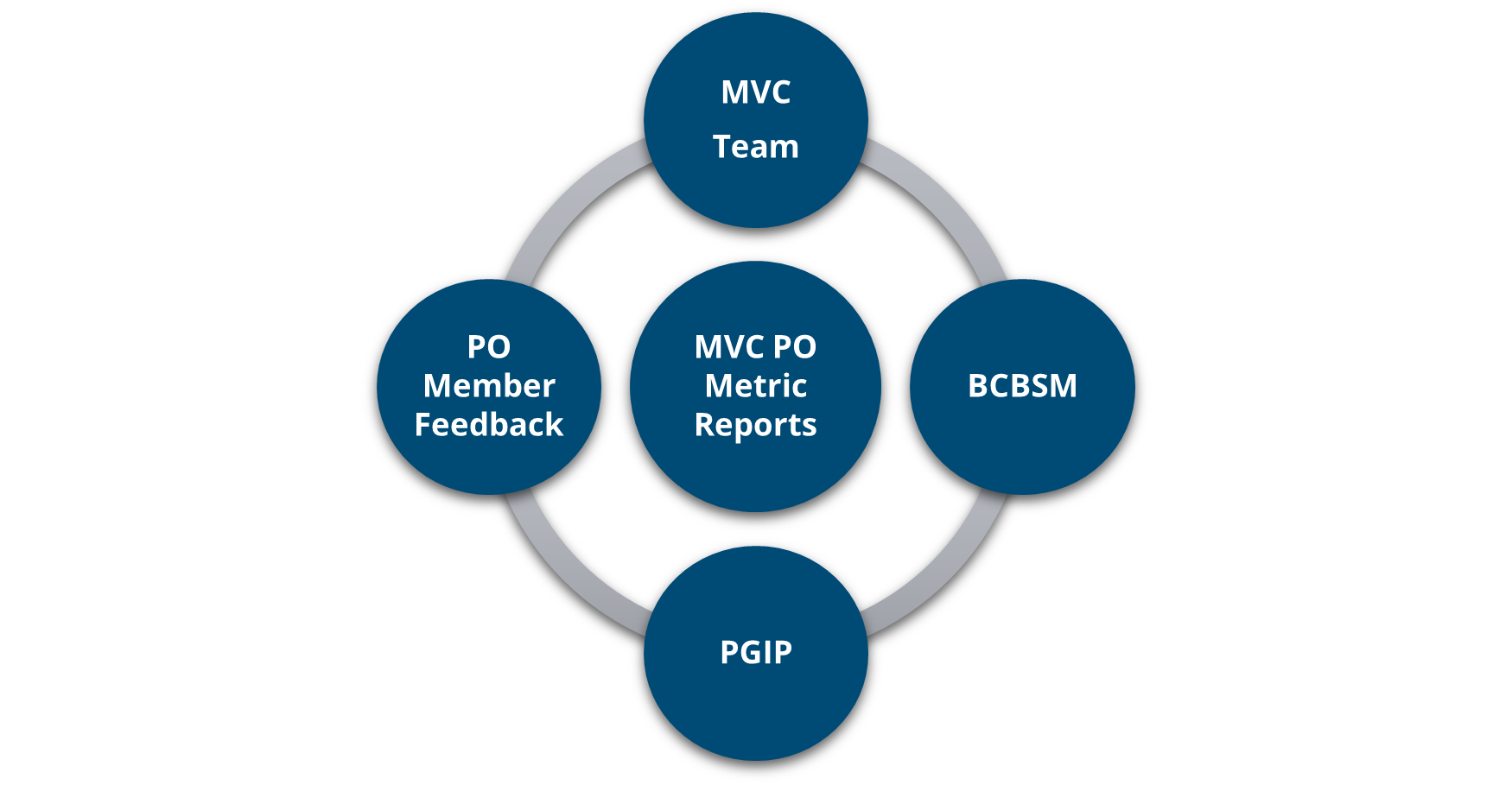
In an effort to provide valuable data to MVC POs, the Coordinating Center continually meets with key stakeholders, BCBSM, and PO members to drive MVC PO report development. The contents of this report were developed based on that feedback. For example, this report allowed POs to individually compare their organization to new comparison groups.
The comparison groups in the new colectomy report include:
- All MVC POs
- EMPLOYED VS. INDEPENDENT POs: As defined in the BCBSM Physician Group Incentive Program (PGIP) 2021 physician list, POs with greater than 50% of their aligned providers employed by a health system are considered employed, and those with less than 50% are considered independent.
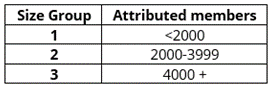
- PO SIZE: These groups were based on the number of attributed members at each PO (Figure 4). Member POs would see the PO size comparison group in which they belong so they can compare their performance to other POs of a similar size.
Figure 4. PO Size Grouping
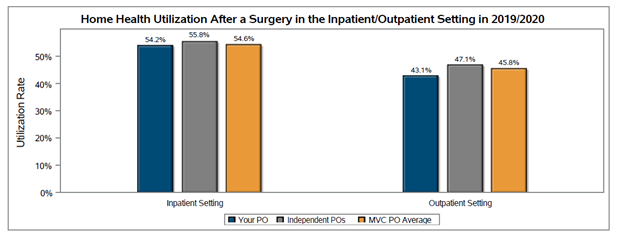
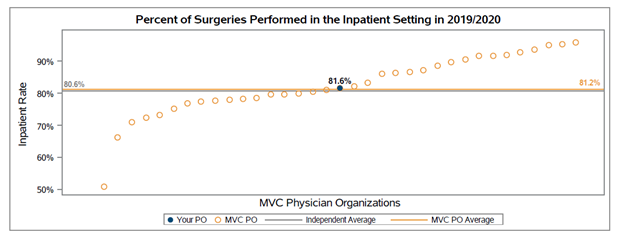
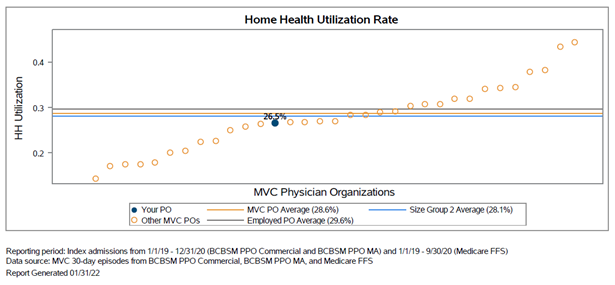
Other components included in the report were a list of the top 10 facilities where a PO’s attributed patients had a colectomy performed, the five most common comorbidities among attributed colectomy patients, median length of stay, 30-day risk-adjusted total episode payment, 30-day readmission rate, and the utilization rate for post-acute care services (emergency department, skilled nursing facility, and home health). General findings included that diabetes was the most common comorbidity across all colectomies (planned and emergent) performed at POs and was frequently one of the top two comorbidities for individual POs. In addition, home health services had the greatest variation in post-acute care utilization (see Figure 5).
Figure 5. PO A Home Health Utilization Rate
By understanding the needs of MVC PO members regarding present and future patient care improvement activities, MVC will be better able to improve future PO reports. If you are interested in sharing feedback about these new PO reports, have any specific PO analytic requests, are undergoing new PO improvement initiatives, and/or would like more information about MVC, please reach out to the Coordinating Center at michiganvaluecollaborative@gmail.com.