MSQC Helps Hospitals Save $3 Million in Colectomy Post-Discharge Spending
“In combining MVC claims data with MSQC abstracted data, it became apparent that readmissions decreased by around 35% between 2018 and 2020 for an estimated cost savings of approximately $2.7 million.”
Background
The Michigan Surgical Quality Collaborative (MSQC) is a statewide initiative dedicated to transforming the quality and cost-effectiveness of surgical care. Using clinical data and expertise from participating hospitals, MSQC hosts a robust registry that provides a rich source of data used to analyze issues, identify best practices, and respond quickly to cost and quality issues.
Over the past several years, MSQC’s quality improvement (QI) projects have supported its participating hospitals in reducing readmissions and emergency department (ED) visits for colectomy patients. This work was partially driven by an increase in readmissions from 2016 to 2018, along with other factors such as variation in rates between sites and existing MSQC quality improvement opportunities in this area. To help estimate the cost savings to payers from reductions in post-discharge care utilization, the MSQC Coordinating Center reached out to the Michigan Value Collaborative (MVC) to establish a baseline and help estimate the value of MSQC’s collaborative activity. The MVC team utilized its robust multi-payer claims data sources to calculate the average costs associated with both readmissions and ED visits following single colectomy episodes.
Methodology
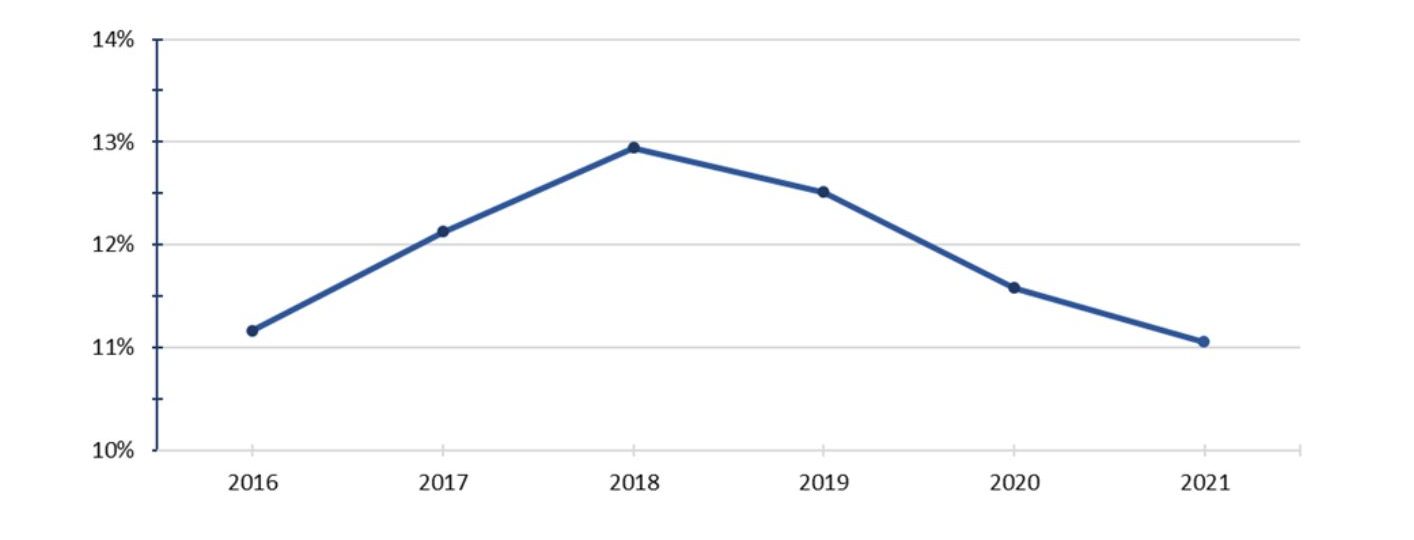
At the outset of this analysis, post-discharge care utilization for 30 days after the surgical event was abstracted from the medical record by trained MSQC data abstractors. The MSQC Coordinating Center then analyzed the sampled and abstracted colectomy readmission and ED visit data from 1/1/16 through 12/31/2021 for the following payers: Medicare Fee-for-Service (FFS), Blue Cross Blue Shield of Michigan (BCBSM) PPO Commercial and Medicare Advantage (MA), and Blue Care Network (BCN) HMO Commercial and MA. Examples of this data can be found in Figure 1. MVC provided data to MSQC representing the standard payments per episode by patient and event, and standard facility payments for post-acute care utilization by payer. The MVC analysis was based on statewide colectomy care claims data from 1/1/16 through 1/31/21 for Medicare FFS, BCBSM PPO (Commercial and MA), and BCN HMO (Commercial and MA).
Limitations
MVC claims data for 30-day readmissions are based on the date of index hospitalization discharge, whereas the MSQC 30-day readmission timeframe is based on the operation date. Since many MSQC hospitals abstract sampled cases, all colectomy cases are not reflected in the MSQC data. Furthermore, patients may have multiple ED visits and readmissions at the same or a different hospital, which may not be included in the MSQC data if the data abstractor is not aware of all visits. In addition, these visits may not always be reflected in MVC data if they are incorporated into a bundled claim with the index surgical event.
It is also important to note that the analysis includes data on healthcare utilization that occurred during the initial years of the COVID-19 pandemic. MSQC data shows a drop in the number of readmissions and ED visits in 2020, which may have been influenced by COVID-related healthcare restrictions and changes in patient behavior. The number of patients with readmissions and ED visits then increased in 2021, possibly related to restored comfort in returning to the healthcare setting.
Timeline of MSQC Quality Initiatives
MSQC incorporated aspects of readmission and ED visit reduction into its annual QI projects over the past several years (including a yearly focus on the colectomy patient population), with the aim of impacting the value of healthcare utilization for colectomy patients in Michigan. In 2017, MSQC sites performed in-depth case analyses on readmissions to identify future performance improvement interventions. Also in 2017, several sites actively participated in an MSQC-facilitated ED visit workgroup to identify and share successful implementation strategies related to the site’s specific QI initiative. In addition, sites must have demonstrated a statistically and clinically significant improvement on one or more high-priority QI target measures (which included readmissions) as a result of a specific process change. Several sites opted to focus on colectomy in 2017.
As part of MSQC’s 2018 QI initiative, sites were required to focus on reducing at least one utilization measure at their facility (e.g., length of stay, ED visits, readmissions) for a focused population, including elective colectomy.
An option for the 2019 QI initiative included the development and implementation of a colectomy care pathway that incorporated several ERAS protocols, which are known to have a positive effect on length of stay without adversely affecting readmissions and ED visit rates.
The 2020 QI initiative focused on pain management and opioid prescribing for selected surgical procedures; colectomy was one of the procedure group options the sites could choose. Educating the patient about pain management strategies in the pre- and post-operative phases and implementing the use of multimodal pain management therapies are essential approaches to help reduce ED visits related to pain.
In 2021, certain sites with baseline data indicating opportunities for improvement could select the QI initiative focused on colorectal cancer (CRC), which included implementing several evidence-based practices from the colorectal care pathway for CRC patients.
Findings & Next Steps
In combining MVC claims data with MSQC abstracted data, it became apparent that readmissions decreased by around 35% between 2018 and 2020 for an estimated cost savings of approximately $2.7 million. This was based on MVC estimates which indicate that if a hospital can reduce the incidence of readmissions within 30 days after discharge, it will save on average $19,184 for each readmission prevented; the readmission rate decreased steadily in MSQC member hospitals from 2018-2021 (see Figure 1). Similarly, avoidance of an ED visit can save $2,239 (averaged across the three payer categories). From 2018-2020, ED visits fell by 20%, delivering associated cost savings of approximately $155k.
Figure 1. Average 30-day post-colectomy readmission rate by year for Medicare, BCBSM, and BCN combined based on MSQC abstracted data
This analysis demonstrated that, in combination with MSQC’s focus on readmissions outcomes and ED visits into several QI projects, progress was made to reduce readmissions and ED visits, especially in 2018 – 2020. This impact may be more significant than presented since MSQC data is limited to sampled cases only.
For next steps, the 2022 MSQC QI initiative requires participating hospitals to submit a root cause analysis on all ED visits related to the principal surgical procedure. This will aid in identifying the underlying reasons behind patients returning to the ED. Sites can then apply this information and implement strategies to reduce avoidable returns to the ED. MSQC’s focus in this area will continue moving forward.