Michigan Bariatric Surgery Collaborative Helps Save $12.5 Million in Opioid Prescription Spending
“The average amount of opioids received in 30-day post-surgery outpatient prescriptions decreased from 297.0 MME in 2015 to 65.4 MME in 2021… Hospitals who participated in the FUTURE enhanced recovery initiative saw the rate of patients receiving opioid amounts above 75 MME decrease more sharply than the rate at other hospitals.”
Background
The Michigan Bariatric Surgery Collaborative (MBSC) is a regional group of hospitals and surgeons that perform bariatric surgery in Michigan. Formed in 2005, MBSC aims to innovate the science and practice of metabolic and bariatric surgery through comprehensive, lifelong, patient-centered obesity care in Michigan and across the United States. Since 2017, MBSC has been working to reduce opioid utilization and prescribing following bariatric surgeries across the state of Michigan. One way in which the MBSC Coordinating Center achieves this reduction is through an opioid value-based metric that aims to reduce new persistent opioid use following surgery. Using annual patient surveys, MBSC is tracking progress toward a collaborative-wide goal of a 2.5% relative reduction in new persistent opioid use (NPOU) per year from baseline to one year after bariatric surgery. Through this effort, the NPOU rate has decreased from 10.4% in 2006 to 3.5% in 2021.
Since 2018, MBSC has also led a voluntary enhanced recovery initiative (Finding Useful Techniques to Upgrade Recovery Enhancement – FUTURE) at five participating hospitals in Michigan. The initiative incorporates evidence-based guidelines for pre-, peri-, post-operative, and post-discharge care to optimize recovery for bariatric surgery patients. The guidelines include a recommendation of prescribing no more than 75 morphine milligram equivalents of oral opiate following surgery. This recommendation is consistent with surgery-specific guidelines set by the Michigan Opioid Prescribing Engagement Network (OPEN).
To help evaluate the impact of its opioid reduction work, the MBSC Coordinating Center reached out to the Michigan Value Collaborative (MVC) in July 2022 to help assess claims-based prescription fills for opioid medications following bariatric surgery. The goal of this analysis was to estimate the overall impact on opioid prescription fills following bariatric surgery in Michigan.
Methodology
Data Sources & Study Population
This analysis used MVC bariatric surgery episodes for Roux-en-Y Gastric Bypass (RYGB) or sleeve gastrectomy hospitalizations, focusing on index admissions between 2015 and 2021. In doing so, 90-day episodes of care were created from claims data for Blue Cross Blue Shield of Michigan (BCBSM) PPO Commercial and Medicare Advantage plans, along with outpatient prescription fill claims data and monthly insurance membership files. The study population was limited to patients with bariatric surgery episodes with continuous enrollment in a prescription sub-plan for 30 days post-surgery and with a bariatric surgery admission date between 1/1/15 and 12/31/21 (n=5,929).
Methodological Approach
Outpatient prescription claims for this cohort were used to identify prescription fills for opioid medications per a comprehensive list of opioid National Drug Codes from the Centers for Disease Control and Prevention (CDC). Receipt of opioids was measured from the bariatric surgery hospital admission date through the following 30 days. Across the 30-day window, the MVC team assessed the rate of any opioid receipt (yes/no), the total amount of opioids received in filled prescriptions, and the percentage of patients who received an amount of opioids above the recommended threshold of 75 MME (equivalent to 10 5mg oxycodone tablets). Rates were calculated overall and stratified by hospital participation in the MBSC enhanced recovery initiative. The opioid amount was assessed in terms of MME using the CDC’s conversion factors and methodology.
To assess the impact of MBSC opioid reduction initiatives on dollars spent by insurance providers, all prescriptions in the 360 days post-bariatric surgery for this cohort were identified and insurance provider payments for those prescriptions were totaled. Average total prescription payments in the 360-day window were compared between patients who received over and under 75 MME opioids post-surgery. The between-group difference in average prescription payments was used in conjunction with annual Michigan bariatric surgery volume and across-year difference in opioid over-prescribing rates to estimate the annual amount of dollars saved by insurance providers.
Limitations
Findings were generated using data for BCBSM PPO and MA patients with a prescription insurance sub-plan, who may differ from the larger Michigan bariatric surgery population. In addition, there may be unseen medication costs or patient factors not captured in this analysis. Estimates of dollars saved assume consistent opioid prescribing rates and bariatric surgery case volumes by year, and no change in prescription costs over time.
Results
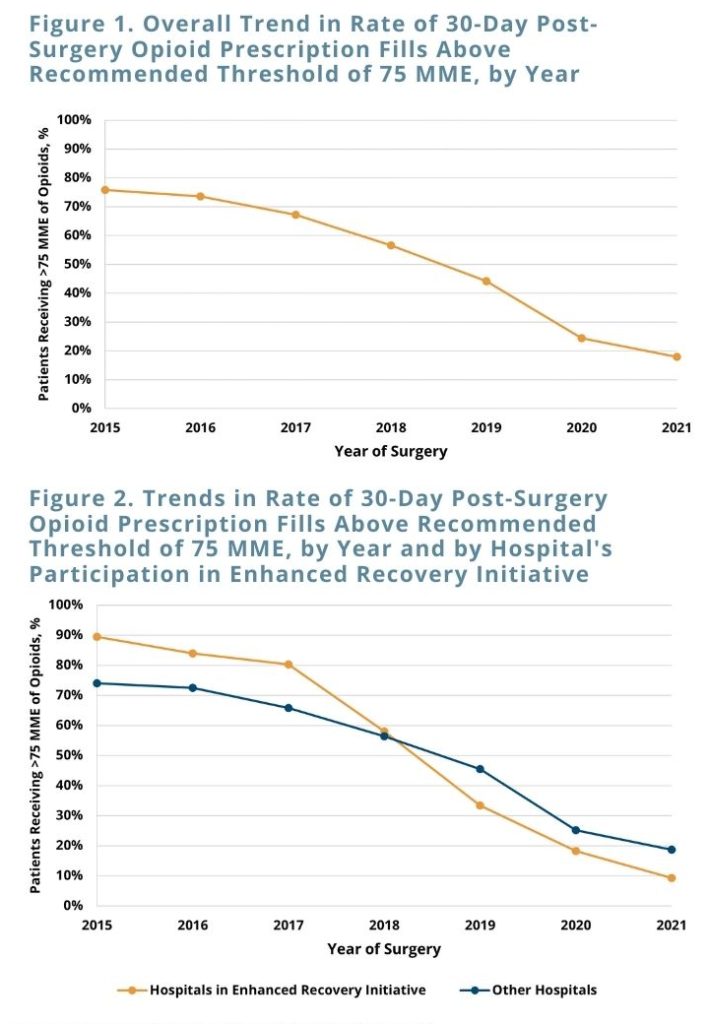
Overall, 73.4% of bariatric surgery patients with RYGB and sleeve gastrectomy episodes in 2015-2021 filled an outpatient opioid prescription in the 30 days post-surgery. The average amount of opioids received in 30-day post-surgery outpatient prescriptions decreased from 297.0 MME in 2015 to 65.4 MME in 2021, and the percentage of patients receiving more than the recommended threshold of 75 MME decreased from 75.8% to 17.9% of bariatric surgery patients (see Figure 1). Hospitals that participated in the FUTURE enhanced recovery initiative saw the rate of patients receiving opioid amounts above 75 MME decrease more sharply than the rate at other hospitals (p=0.02) (see Figure 2).
Insurance providers spent an average of $978 more on all prescription medications per patient in the year following bariatric surgery for patients who were over-prescribed opioids compared to patients who received up to 75 MME. From 2015 to 2021, MBSC’s targeted opioid reduction activity contributed to a 57.9% decrease in the statewide post-bariatric surgery opioid overprescribing rate. For Michigan bariatric surgeries in 2016 through 2021, yearly decreases in opioid over-prescribing rates compared to the rate in 2015 resulted in an estimated $12.5 million dollars saved on prescription payments in the 360 days post-surgery. This calculation of dollars saved is compared to the estimated amount that would have been spent by insurance providers on post-surgery prescription medications if the statewide opioid over-prescribing rate had remained constant from 2015 onwards. Savings on prescription payments associated with opioid reductions can be attributed to decreased opioid payments as well as to the prevention of downstream health effects that may be caused by opioids. Analyses indicate that yearly savings would continue to increase thanks to reductions in the over-prescribing rate following bariatric surgery.
Conclusions & Next Steps
MBSC’s recent efforts in post-bariatric surgery opioid reduction were associated with significant decreases in opioid overprescribing rates, particularly at hospitals participating in MBSC’s FUTURE initiative. In addition to saving $12.5 million from 2016 – 2021, opioid reduction following Michigan bariatric surgeries is estimated to save insurance payers over $4.3 million dollars annually in prescription payments in future years.
There is a wealth of evidence supporting the positive impact of opioid reduction on the health of Michigan bariatric surgery patients. MVC also found decreased emergency department utilization and hospital readmissions for patients who received a recommended dose of opioids compared to those who filled prescriptions greater than 75 MME. MBSC found that new persistent opioid use – which is associated with increased healthcare spending (Lee, 2020) – was more common following bariatric surgery for patients who received greater than 75 MME compared to those who received up to 75 MME (rate of 3.7% compared to 3.53%). A reduction in opioid overprescribing is expected to prevent cases of opioid use disorder, which the CDC estimates costs nearly $18 billion dollars per year in Michigan (Luo, 2021). Efforts like those of MBSC are effective in reducing costs and improving outcomes following bariatric surgery.