Assessing the Impact of Bariatric Surgery on Diabetes Medication Prescription Fills in Michigan
Background
The Michigan Bariatric Surgery Collaborative is a regional group of hospitals and surgeons that perform bariatric surgery in Michigan. Formed in 2005, MBSC aims to innovate the science and practice of metabolic and bariatric surgery through comprehensive, lifelong, patient-centered obesity care.
Since its inception, MBSC has worked closely with participants to improve the quality of obesity care through regular data and information sharing. As part of these efforts, the MBSC Coordinating Center reached out to the Michigan Value Collaborative (MVC) Coordinating Center in early 2022 to help assess the impact of bariatric surgery on prescription fills for diabetes medications across the state of Michigan. This request was largely driven by existing evidence in the literature that shows that bariatric surgery has resolved or improved Type 2 diabetes symptoms in a large proportion of patients (Varban et al., 2022). Using its rich administrative claims data sources, the MVC team first analyzed pre-surgery and post-surgery receipt of diabetes medications. This information was then used to estimate a high-level snapshot of the overall impact across Michigan. MVC’s analysis included estimated cost savings to health insurance providers that could be attributed to a decrease in post-surgery diabetes medication prescription fills.
Methodology
Data Sources & Study Population
The analysis conducted used bariatric surgery episodes for Roux-en-Y Gastric Bypass (RYGB) and sleeve gastrectomy hospitalizations, focusing on index admissions between 2015 and 2021. In doing so, 90-day episodes of care were created from claims data for Blue Cross Blue Shield of Michigan (BCBSM) PPO Commercial and BCBSM Medicare Advantage plans. Prescriptions filled pre- and post-surgery were assessed using paid outpatient prescription claims, and monthly BCBSM membership files were used to ensure patients’ continuous enrollment in a prescription insurance sub-plan during the follow-up window.
The study population was limited to patients with bariatric surgery episodes who had a diagnosis of Type 2 diabetes in the 180 days prior to surgery and filled an outpatient prescription for diabetes medication in the 120 days prior to their discharge. The cohort was further limited to individuals within BCBSM membership files who were continuously enrolled in a prescription sub-plan for 120 days prior to surgery and 120 (n=899), 240 (n=760), or 360 (n=635) days post-surgery.
Methodological Approach
Diabetes medications were identified in outpatient prescription medication claims using National Drug Codes and medication names. Medications were then grouped by drug class and categorized as insulin, GLP-1 RA, or other oral diabetes medications. Prescription fills were assessed by 120-day periods pre- and post-surgery relative to the date of discharge from the index bariatric surgery hospitalization.
Prescription payments were assessed according to the insurance payer’s paid amount on each claim. For each episode, the amount paid by the insurance provider on all diabetes medications in a 120-day period was totaled, then the total amount paid per relative time window was averaged across episodes. This average was then used to extrapolate cost savings across the larger population of patients undergoing bariatric surgery.
Limitations
Payment measures were derived for patients enrolled in BCBSM PPO Commercial and MA prescription sub-plans; although a sensitivity analysis implied alignment with Medicare paid amounts, BCBSM payments may differ from other payer payments for diabetes medications. Furthermore, extrapolating results assumes that the larger population of patients undergoing bariatric surgery have a similar distribution of prescription fills for diabetes medications. Finally, this analysis assumed consistent dollar amounts paid per prescription over time.
Findings
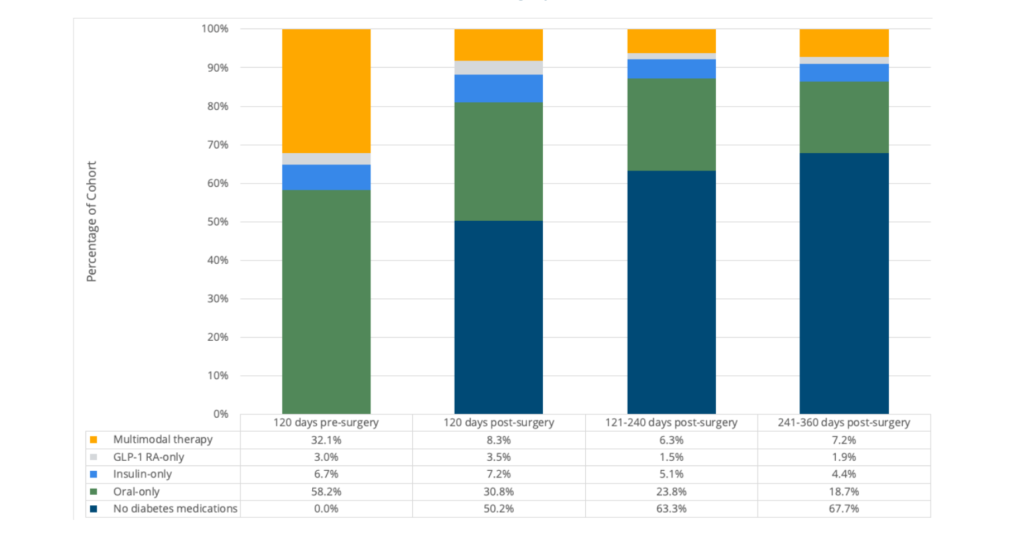
Among a cohort of bariatric surgery patients with Type 2 diabetes who met the criteria described above (n=760), 88% filled an outpatient prescription for an oral diabetes medication, 30% for insulin, and 21% for a GLP-1 RA medication prior to surgery. From the 120 days pre-surgery to the 120 days post-surgery, there was a significant decrease in fills for any diabetes medication (p<.001). The most frequent change in medications between pre-surgery and post-surgery was from oral diabetes medication to no diabetes medication. In the 1 to 120 days following surgery, 50% of patients filled no diabetes medication prescriptions, and in the 121 to 240 days following surgery, 63% of patients filled no diabetes medication prescriptions (see Figure 1).
In the first 360 days following bariatric surgery, there was an average decrease in diabetes prescription payments made by the insurance provider of about $4,133 per PPO patient. With a total of 54,454 bariatric surgeries performed in Michigan between 2015 and 2021, and given that 34% of bariatric surgery patients have diabetes, insurance providers in Michigan saved an estimated $76.5 million on diabetes medications in the 360 days following bariatric surgeries in 2015-2021. Data suggest that savings would continue to increase in the following years post-surgery.
In this population of Michigan bariatric surgery patients with Type 2 diabetes who filled pre-surgery diabetes medication prescriptions, there was a significant decrease in the percentage who filled any diabetes prescription post-surgery. There was also a substantial decrease in average insurance provider payments for diabetes medications from pre-surgery to post-surgery. These results provide evidence of statewide clinical outcome improvement and cost savings for Type 2 diabetes following bariatric surgery.