MUSIC Providers Help Avert Estimated $1.6 Million in Avoided Opioid Prescription Spending After Prostate Surgery
“The change in opioid prescribing resulted in an estimated yearly average savings of $1,132 per patient. These estimates were extrapolated to find a cost savings of over $1.6 million during the period of 2019-2021.”
BACKGROUND
The Michigan Urological Surgery Improvement Collaborative (MUSIC) is a physician-led quality improvement collaborative comprised of a consortium of urology practices across the state of Michigan. MUSIC works to evaluate and improve the quality and cost efficiency of urologic care. Since 2011, MUSIC has led prostate-related quality improvement activities such as improving patterns of care in the radiographic staging of men with newly diagnosed prostate cancer, reducing prostate biopsy-related hospitalizations, and enhancing the appropriateness of treatment decisions. In 2016, MUSIC expanded its scope of work to kidney stone surgery and in 2017 to small renal masses.
The MUSIC Prostate team pursued a variety of tailored initiatives in recent years, one of which worked to optimize pain control following surgery for prostate cancer and to reduce potentially unneeded opioid prescriptions. The Michigan Pain-control Optimization Pathway (MPOP) Initiative aims to help patients recover faster and return to their normal selves while safely limiting, if appropriate, the number of opioid tablets a patient receives following prostate removal surgery. This MPOP Initiative incorporates patient resources on safe pain management after prostate surgery, as well as guidance for providers on an opioid-free prostatectomy pathway. The initial guidelines, introduced in 2018, recommended prescribing no more than 45 morphine milligram equivalents (MME) of oral opiate following surgery, based on research findings that utilized MUSIC’s clinical data (Shah et al., 2020)*. In 2020, these guidelines were updated to recommend zero opioids for prostate cancer surgery patients.
To help understand the quality improvement benefits of its opioid reduction work, the MUSIC team reached out to the Michigan Value Collaborative (MVC) in 2022 to assess how its MPOP Initiative changed claims-based prescription fills for opioid medications following prostatectomy. The goal of this analysis was to estimate the initiative’s overall impact on opioid prescription fills following prostate removal surgery in Michigan and any related cost savings that improved the value of care delivery.
METHODOLOGY
Data Sources & Study Population
MVC prostatectomy episodes were used for this analysis and were limited to those performed by MUSIC providers and Michigan non-MUSIC providers from January 1, 2015 to December 31, 2021. The opioid utilization analysis focused on Blue Cross Blue Shield of Michigan (BCBSM) PPO Commercial and Medicare Advantage (MA) insured patients. After subsetting to BCBSM-insured prostatectomy patients with a prescription sub-plan and continuous enrollment for at least 30 days post-surgery, the cohort included 1,797 patients.
Methodological Approach
The study population was identified using professional claims for MVC prostatectomy episodes that occurred within the index dates of the surgery. All professional claims missing a provider NPI on the claim were excluded. The remaining NPIs were characterized by information derived from the National Plan and Provider Enumeration System (NPPES) dataset. Claims of providers or facilities outside of the state of Michigan were also excluded. The remaining NPIs were then categorized into MUSIC and non-MUSIC categories. Prostatectomies performed by MUSIC providers were categorized using an NPI list provided by MUSIC, and prostatectomies performed by non-MUSIC providers were categorized using an NPI list provided by MUSIC and NPIs of other Michigan urologists, other Michigan providers, or Michigan facilities.
Opioid utilization was assessed through the presence of paid outpatient opioid prescription claims in the 30 days post-surgery. Overutilization was assessed by the proportion of patients exceeding the goal of 45 MME or less after surgery. Opioid utilization was only assessed among BCBSM episodes.
Limitations
There were some limitations to this analysis. First, approximately 90% of Michigan urologists participate in MUSIC. However, only about 63% of all MVC prostatectomy episodes were identified as being performed by a MUSIC provider via National Provider Identifier (NPI). It’s possible that some MUSIC providers are performing prostatectomies on patients with an insurance plan not reflected in MVC data. It could also be related to MVC’s episode structure. Episodes are mutually exclusive; therefore, if a patient were to have a hospitalization prior to their prostatectomy that resulted in an MVC episode creation, their care would not be classified as a prostatectomy episode. It is also possible that billing NPI was not always a reliable field.
Second, MVC only has outpatient prescription claims for BCBSM and BCN patients with a prescription sub-plan. For the purposes of this study, only BCBSM-insured patients were assessed. As a result, only about 20% of MVC prostatectomy episodes were included in assessing opioid utilization. Furthermore, the analysis is of opioid utilization, not provider prescribing patterns. Given that a claim is only generated once a prescription is filled, this analysis cannot provide a full picture of changes in provider prescribing patterns.
RESULTS
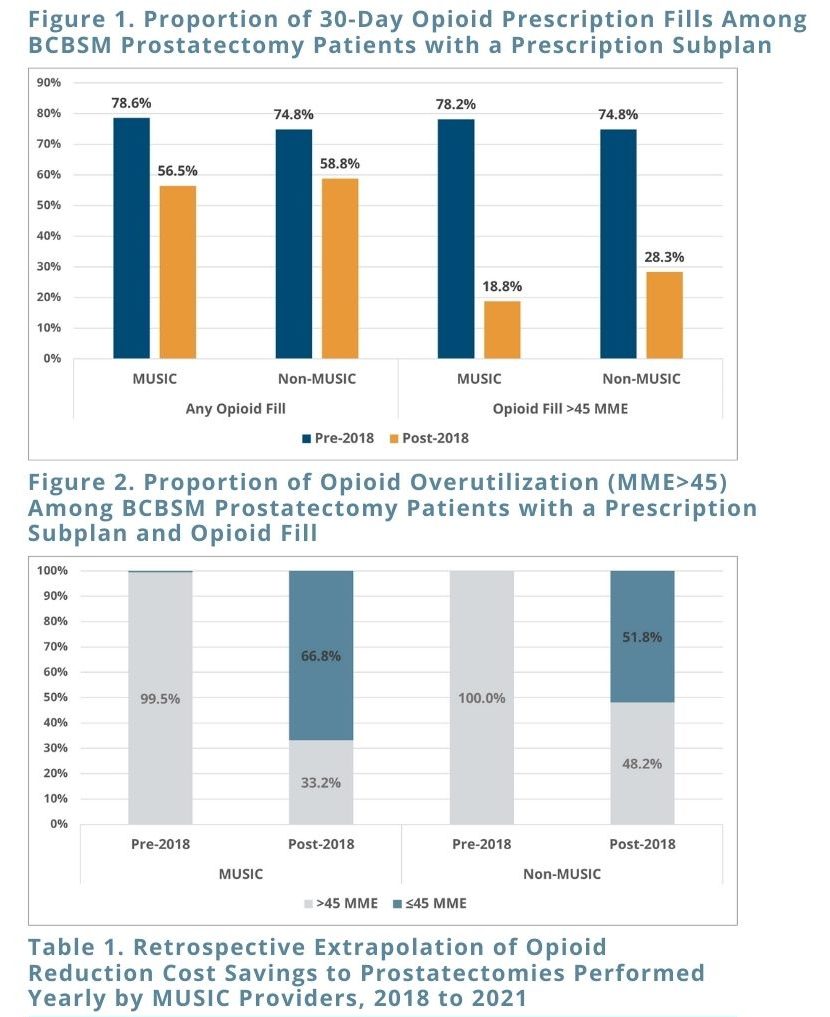
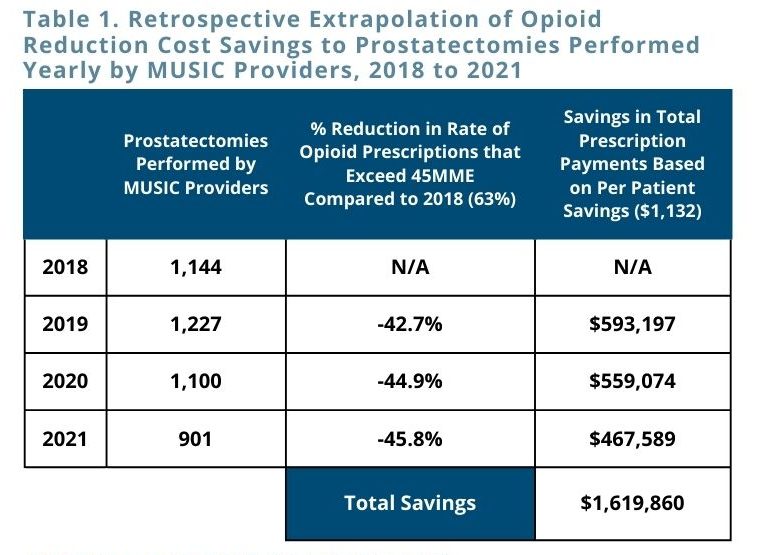
Among the BCBSM-insured prostatectomies performed by MUSIC providers prior to 2018, 78.6% resulted in an opioid fill within 30 days of surgery. Among prostatectomies performed by MUSIC providers after 2018, only 56.5% resulted in an opioid fill (Figure 1). This analysis revealed that opioid utilization patterns among patients whose prostatectomies were performed by MUSIC providers dropped substantially in 2018 and onwards. In addition, although these patterns were similar for non-MUSIC providers, the absolute decrease in opioid prescription fill rates was greater for MUSIC providers. The analysis further revealed that not only did opioid prescription utilization decrease, but the amount filled decreased substantially. Among MUSIC providers, opioid prescriptions went from being greater than the recommended 45 MME 99.5% of the time prior to 2018 to only 33% of the time post-2018 (Figure 2) – a greater decrease than was observed for non-MUSIC providers.
In addition, MVC estimated cost savings from the reduction in opioid prescribing that exceeds the recommended prescription amount by examining differences in prescription expenditures among the MUSIC cohort, comparing those that had an opioid prescription fill of greater than 45 MME to those that had an opioid prescription fill of 45 MME or less. The changes in opioid prescribing resulted in an estimated yearly average savings of $1,132 per patient.
CONCLUSIONS & NEXT STEPS
This analysis demonstrated the impact and value of MUSIC’s MPOP Initiative in reducing opioid prescribing after prostatectomy, with significant decreases in prescribing rates for greater than 45 MME among participating providers. Using the estimated savings of $1,132 per patient, MVC used the number of prostatectomies performed each year by MUSIC providers combined with the yearly percent reduction from baseline in opioid prescribing for greater than 45MME to further estimate a savings of over $1.6 million from avoided opioid prescription payments since 2018 (see Table). There is evidence that MUSIC’s efforts improved value and patient outcomes, with opportunities to further reduce the negative effects of opioid pain medications in the future.